Addiction: The Metabolic Crisis Behind Cravings
You've been told addiction is about hijacked reward circuits. That drugs flood your brain with dopamine and you lose control. That it's a chronic brain disease requiring lifelong management.
That's not wrong. But it misses the point entirely.
Why do some people's reward circuits get hijacked while others don't? Why can one person have a drink and walk away, while another can't stop? Why does stress trigger relapse in some people but not others?
The answer isn't genetics or willpower. It's metabolism.
The Systems That Fail
Addiction happens when multiple metabolic systems break down simultaneously. Not just one thing going wrong—everything going wrong at once.
Here's what's actually happening:
1. Dopamine Pathways Can't Regulate
Dopamine synthesis requires tyrosine, iron, B6, copper, and tetrahydrobiopterin (BH4). When any of these are deficient, dopamine production drops.
Your brain doesn't feel reward from normal activities. Food tastes bland. Accomplishments feel empty. Social connection doesn't satisfy.
Then you try something that bypasses the entire system—alcohol, stimulants, gambling, whatever—and suddenly you feel normal. Not high. Normal.
That's not addiction. That's self-medication for dopamine deficiency.
Studies show people with lower dopamine D2 receptors experience less pleasure from natural rewards and show increased vulnerability to addiction. This isn't genetic destiny—receptor expression changes based on nutrient status, inflammation, and toxic burden.
2. Glutamate-GABA Balance Collapses
Your brain runs on a balance between glutamate (excitation) and GABA (inhibition). Converting glutamate to GABA requires the GAD enzyme, which depends on vitamin B6—specifically the active P5P form.
Up to 30% of people can't efficiently convert regular B6 to P5P. They're functionally B6 deficient even with adequate intake.
Result? Glutamate builds up. GABA drops. You're stuck with the accelerator pressed and the brakes failing.
That feels like anxiety, insomnia, racing thoughts, inability to relax. Alcohol works as an NMDA receptor antagonist, blocking glutamate and enhancing GABA. For someone with glutamate-GABA imbalance, alcohol doesn't just feel good—it provides neurochemical relief they can't get any other way.
Again: not addiction. Self-medication.
3. Mitochondria Stop Producing Enough Energy
Neurotransmitter synthesis requires ATP. Dopamine synthesis needs energy. GABA synthesis needs energy. Serotonin synthesis needs energy.
When mitochondrial function declines due to oxidative stress, nutrient deficiencies, or chronic inflammation, ATP production drops. Your neurotransmitter systems start running on empty.
The reward system becomes hypersensitive because it's energy-starved. Small hits of external dopamine (from substances or behaviors) create disproportionate responses because the system is so depleted.
Studies show people with chronic fatigue and mitochondrial dysfunction have significantly higher rates of addiction. Not because they're weak-willed—because their brains literally don't have the energy to maintain normal reward function.
4. Heavy Metals Disrupt Everything
Mercury doesn't just "damage neurons." It increases striatal dopamine to 907% of baseline at moderate concentrations. It inhibits glutamate uptake by astrocytes to 46% of control levels. It triggers chronic neuroinflammation through microglial activation.
Here's where it gets interesting: alcohol produces a 10-fold increase in mercury vapor exhalation and corresponding reduction in tissue mercury accumulation. Animal studies consistently demonstrate alcohol's protective effects against inorganic mercury toxicity.
Could alcoholism in some people represent a biological response to chronic mercury exposure? The mechanistic evidence is compelling. The epidemiological validation is missing. But the hypothesis deserves investigation.
Lead, cadmium, and other heavy metals compound these effects. Lead exposure increases impulsivity and reduces impulse control. Cadmium disrupts zinc metabolism, which affects hundreds of enzymes including those involved in neurotransmitter regulation.
5. Serotonin System Breaks Down
Your gut produces 90% of your body's serotonin. When you have gut dysbiosis, leaky gut, or chronic inflammation, serotonin production plummets.
Serotonin synthesis requires tryptophan, B6, folate, B12, iron, and magnesium. Deficiency in any of these creates problems.
Low serotonin manifests as depression, poor sleep, carbohydrate cravings, and mood instability—all of which correlate strongly with addiction vulnerability.
6. Neuroinflammation Becomes Chronic
Inflammatory cytokines directly interfere with neurotransmitter metabolism. They reduce dopamine synthesis, increase glutamate, decrease GABA, and impair serotonin production.
Inflammation comes from multiple sources: gut dysbiosis, food sensitivities, chronic infections, toxic burden, psychological stress. It creates a state of chronic neurochemical dysfunction.
Interestingly, moderate alcohol consumption promotes an anti-inflammatory microglial phenotype, increasing IL-10 and TGF-β without elevating pro-inflammatory markers. This anti-inflammatory effect could provide relief from mercury-induced or other sources of neuroinflammation.
The Cumulative Effect
When all these systems fail simultaneously, you don't have "an addictive personality." You have:
- Dopamine deficiency making natural rewards feel meaningless
- Glutamate excess creating anxiety and inability to relax
- Energy crisis making everything harder
- Toxic burden disrupting neurotransmitter regulation
- Serotonin depletion causing depression and mood instability
- Neuroinflammation compounding all the above
In this metabolic environment, substances or behaviors that temporarily normalize these systems feel like survival, not recreation.
Why the Disease Model Fails
The "chronic brain disease" model treats addiction as the primary problem. But what if addiction is the adaptive response to underlying metabolic dysfunction?
Consider: studies of addiction treatment show 40-60% relapse rates within the first year. Why? Because detox and behavioral therapy don't address the metabolic conditions that created vulnerability in the first place.
You can't willpower your way out of dopamine deficiency. You can't therapy away glutamate excess. You can't motivational-interview mitochondria into producing more ATP.
The relapse isn't a failure of recovery. It's the body seeking neurochemical homeostasis through the only pathway it knows works.
What Actually Works
If addiction reflects metabolic dysfunction, then metabolic restoration should reduce cravings. Does it?
Dopamine Support
Tyrosine is the precursor to dopamine. Studies show tyrosine supplementation improves cognitive function during stress and reduces subjective fatigue.
But tyrosine alone isn't enough. You need:
- Iron (15-25mg daily for deficiency; test first) - required for tyrosine hydroxylase
- B6 (P5P) (25-50mg daily) - required for aromatic amino acid decarboxylase
- Copper (1-2mg daily) - required for dopamine beta-hydroxylase
- Folate (methylfolate 400-800mcg) - required for BH4 synthesis
- B12 (methylcobalamin 1000mcg) - cofactor in multiple pathways
Glutamate-GABA Balance
P5P supplementation directly supports GAD enzyme function, increasing GABA synthesis. Use 50-100mg daily.
Magnesium blocks NMDA receptors, preventing glutamate excitotoxicity. 400-600mg daily (glycinate, threonate, or malate forms).
Zinc modulates glutamate receptors and helps activate GAD. 15-30mg daily with 1-2mg copper to prevent imbalance.
Taurine (500-3000mg daily) - modulates GABA receptors directly. L-theanine (200-400mg) - increases GABA and reduces glutamate.
Mitochondrial Support
ATP production requires specific nutrients:
- CoQ10 (100-300mg daily) - electron transport chain
- PQQ (10-20mg daily) - mitochondrial biogenesis
- Alpha-lipoic acid (300-600mg daily) - antioxidant, energy production
- B-complex with all eight B vitamins in active forms
- Magnesium (overlaps with glutamate support)
Glutathione Pathway
Glutathione protects against oxidative stress and binds toxins for elimination. It requires:
- NAC (1200-1800mg daily) - provides cysteine
- Glycine (3-5g daily) - often limiting factor
- Selenium (200mcg daily) - required for glutathione peroxidase
Serotonin Support
Support gut health to restore serotonin production:
- Multi-strain probiotics (Lactobacillus and Bifidobacterium)
- L-glutamine (5-15g daily) for gut lining repair
- Tryptophan (500-2000mg) or 5-HTP (50-300mg) - serotonin precursors
- Address food sensitivities and inflammation
Anti-Inflammatory Support
Reduce neuroinflammation:
- Omega-3s (EPA+DHA 2-4g daily)
- Curcumin (500-2000mg daily with piperine)
- Vitamin D (optimize to 50-70 ng/mL)
- Eliminate inflammatory triggers (processed foods, excess sugar, gut irritants)
Detoxification
For mercury and other heavy metals:
- Safe chelation protocols using DMSA or DMPS (under medical supervision)
- Nutritional support before chelation (selenium, zinc, glutathione pathway nutrients)
- Gut function optimization (bile flow, regular bowel movements)
- Sauna therapy for mobilization and elimination
See Mercury Detox and Nutritional Detox for detailed protocols.
The Tiered Approach
Tier 1: Foundation (Everyone Starts Here)
- P5P 50mg
- Magnesium glycinate 400-600mg
- Zinc 15-30mg with copper 1-2mg
- B-complex (methylated forms)
- Vitamin D optimization
Tier 2: Glutathione & Energy Support
- NAC 1200-1800mg
- Glycine 3-5g
- CoQ10 100-300mg
- Alpha-lipoic acid 300-600mg
- Selenium 200mcg
Tier 3: Neurotransmitter Targeting
- Tyrosine 500-2000mg (morning)
- Taurine 1000-3000mg
- L-theanine 200-400mg
- 5-HTP or tryptophan (evening)
Tier 4: Detoxification & Advanced
- Mercury testing and safe chelation
- Gut microbiome optimization
- Mitochondrial support (PQQ, carnitine)
- Inflammation resolution (omega-3s, curcumin)
Non-Negotiables
Supplements alone won't fix everything. These are essential:
Sleep: Sleep deprivation increases glutamate and disrupts dopamine signaling. 7-9 hours non-negotiable.
Stress Management: Cortisol increases glutamate release and depletes GABA. Find sustainable stress reduction.
Exercise: Moderate exercise supports dopamine, reduces inflammation, improves mitochondrial function. But excessive exercise is a stressor.
Sunlight: Light exposure regulates circadian rhythm, supports vitamin D, influences neurotransmitter production.
Connection: Isolation worsens metabolic dysfunction. Social connection is neurochemical medicine.
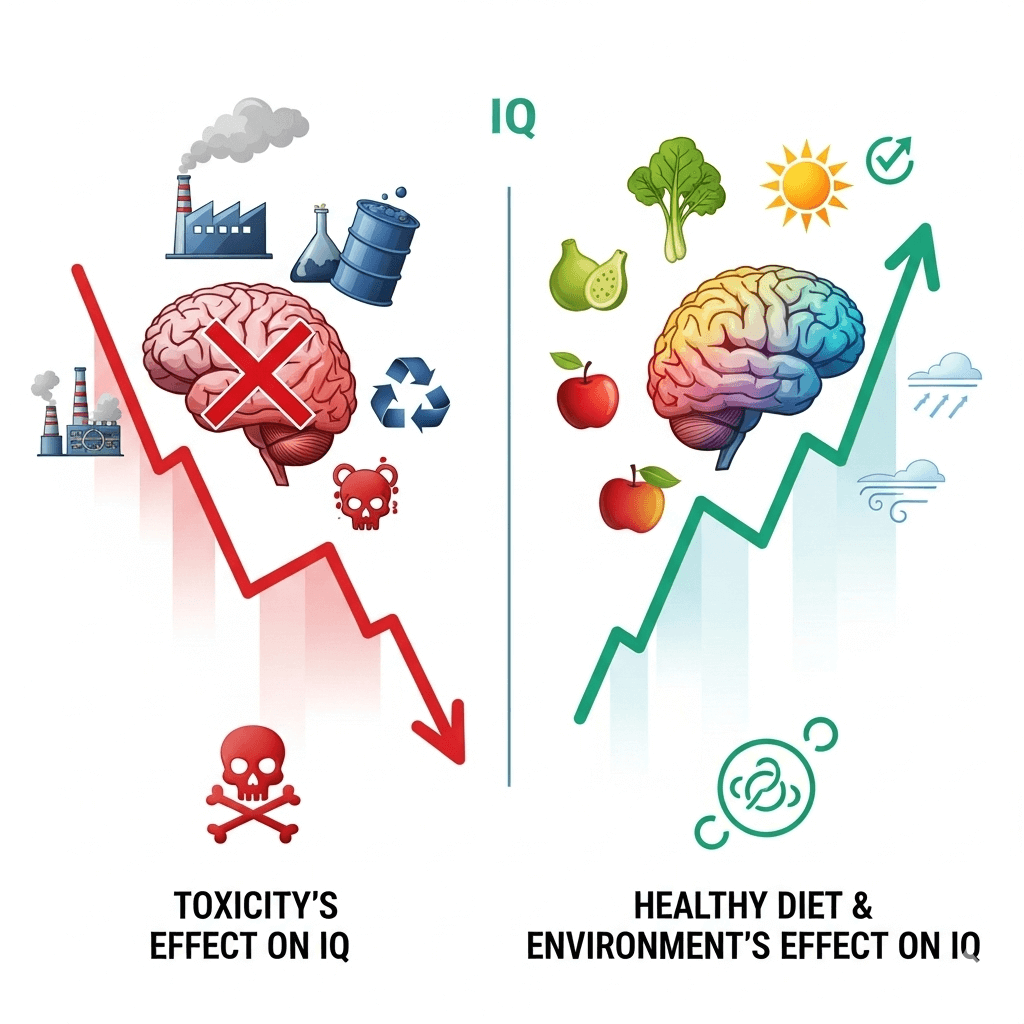
The Genetics Question
"But addiction runs in my family. Isn't it genetic?"
Yes, genetic variants affect neurotransmitter metabolism. COMT variants affect dopamine clearance. GAD1 variants affect GABA synthesis. MTHFR variants affect methylation and neurotransmitter production.
But genetics operate within a metabolic context.
Someone with "bad" genetics but optimal nutrients, low inflammation, minimal toxic burden, and good gut health? Often minimal symptoms.
Someone with "good" genetics but severe nutrient deficiencies, chronic stress, gut dysfunction, and high toxic load? Significant vulnerability.
Genes load the gun. Environment pulls the trigger.
More accurately: environment determines whether there are bullets in the gun at all.
Why Avoidance Isn't Enough
Can you just avoid addictive substances? Sure. But you're not addressing the metabolic dysfunction driving the cravings.
You'll still have:
- Anhedonia (inability to feel pleasure)
- Anxiety from glutamate excess
- Fatigue from mitochondrial dysfunction
- Depression from serotonin depletion
- Inflammation driving neurochemical chaos
That's called "dry drunk syndrome" in alcoholism recovery. You're not drinking, but you're miserable because the underlying metabolic problems remain.
Sobriety without metabolic restoration isn't recovery. It's white-knuckling through biological dysfunction.
Real Recovery
Real recovery means restoring the systems that regulate reward, mood, energy, and stress response.
It means:
- Dopamine pathways that respond to natural rewards
- Glutamate-GABA balance that allows relaxation without substances
- Mitochondria producing adequate ATP for neurotransmitter synthesis
- Toxic burden reduced to manageable levels
- Gut producing serotonin normally
- Inflammation under control
When these systems work properly, cravings diminish. Not through willpower—through biochemistry.
My Approach
I don't think about addiction as a disease to manage. I think about it as metabolic dysfunction to correct.
Foundation: P5P, magnesium, zinc, B-complex, vitamin D Glutathione pathway: NAC, glycine, selenium Energy support: CoQ10, alpha-lipoic acid, PQQ Neurotransmitter precursors: Tyrosine (morning), taurine, L-theanine Gut health: Probiotics, L-glutamine, addressing sensitivities Detox: Tested mercury, following safe chelation protocols Lifestyle: Sleep priority, sunlight, moderate exercise, stress management
Result? The substances or behaviors that once felt necessary lose their pull. Not because of willpower. Because the systems they were compensating for now work properly.
That's not managing a chronic disease. That's fixing broken metabolism.
The Bottom Line
Addiction isn't about hijacked reward circuits. It's about multiple metabolic systems failing simultaneously and the body's desperate attempt to restore homeostasis through whatever works.
Dopamine deficiency. Glutamate excess. Energy crisis. Toxic burden. Serotonin depletion. Neuroinflammation.
Fix those, and addiction often resolves. Not always completely. Not always quickly. But consistently enough that the metabolic model deserves serious consideration.
This isn't genetic determinism. It's metabolic biochemistry. And unlike your genes, your metabolism is modifiable.
Addiction is metabolic dysfunction looking for chemical homeostasis. Give your body what it actually needs, and the cravings for what it doesn't often disappear.
Further Reading
- Addiction Research - Comprehensive literature review
- Addiction Recovery Protocols - Detailed tiered approach
- Mercury & Alcoholism - Specific mercury-alcohol connection
- Free Glutamate - Glutamate-GABA balance in depth
- Dopamine Metabolism - Dopamine synthesis pathways
- Gut-Brain Axis - Gut health and neurotransmitters