Root Causes of Addiction: A Systems View
Addiction doesn't happen because someone lacks willpower or made poor choices. It emerges when multiple metabolic systems fail simultaneously, creating a biochemical environment where substances become the only reliable way to feel normal. Understanding which specific systems are broken in your case is the key to personalized recovery.
When Multiple Systems Fail Together
The person who drinks occasionally and never develops a problem has functional dopamine synthesis, adequate GABA production, efficient detoxification, and resilient mitochondria. The person who becomes addicted after a few exposures often has several systems already compromised: perhaps depleted dopamine from chronic stress, impaired GABA synthesis from vitamin B6 deficiency, accumulated mercury toxicity from dental amalgams, and mitochondrial dysfunction from years of poor diet.
The substance didn't create these problems—it revealed them. More precisely, it temporarily masked them while making them progressively worse.
Individual variation is profound. Some people have genetic variants affecting dopamine metabolism (COMT, MAO). Others have gut dysfunction preventing serotonin synthesis. Still others carry heavy metal burdens that directly interfere with neurotransmitter production. Many have all of these simultaneously, creating compounding vulnerability.
This article provides a framework for identifying which systems are most compromised in your specific case, allowing you to design a targeted restoration protocol rather than guessing or following generic approaches.
Dopamine System Dysfunction
Dopamine is your brain's primary reward and motivation neurotransmitter. When dopamine synthesis is impaired or receptors are damaged, nothing feels rewarding anymore—except substances that artificially spike dopamine levels.
The Synthesis Pathway
Dopamine synthesis requires a multi-step pathway with specific nutrients at each stage:
-
Tyrosine → L-DOPA: Catalyzed by tyrosine hydroxylase, which requires iron and tetrahydrobiopterin (BH4). BH4 synthesis itself needs folate, B2, B3, and magnesium. Many people are deficient in iron, particularly women and those with gut malabsorption, creating a bottleneck at the very first step.
-
L-DOPA → Dopamine: Catalyzed by aromatic amino acid decarboxylase (AADC), which has an absolute requirement for pyridoxal-5-phosphate (P5P), the active form of vitamin B6. Without adequate P5P, this conversion fails.
-
Dopamine → Norepinephrine: Some dopamine converts to norepinephrine via dopamine beta-hydroxylase, which requires copper and vitamin C. Copper deficiency (common with zinc supplementation or high copper-depleting foods) impairs this pathway.
Dopamine Breakdown and COMT Variants
Once synthesized, dopamine must be metabolized. The primary enzyme is catechol-O-methyltransferase (COMT), which requires magnesium and SAMe (from methylation). COMT has well-studied genetic variants:
- COMT Met/Met (slow): Breaks down dopamine slowly, leading to higher baseline dopamine but vulnerability to overstimulation, anxiety, and difficulty handling stress.
- COMT Val/Val (fast): Breaks down dopamine rapidly, leading to lower baseline dopamine, reward deficiency, and higher addiction vulnerability.
- COMT Val/Met (intermediate): Balanced breakdown.
People with fast COMT variants often feel chronically unrewarded and are drawn to stimulants (cocaine, methamphetamine, nicotine) or activities that spike dopamine (gambling, risk-taking). They may also benefit more from substances that slow dopamine breakdown.
D2 Receptor Downregulation
Chronic substance use causes dopamine receptors (particularly D2 receptors) to decrease in number and sensitivity—a protective response to unnaturally high dopamine levels. This downregulation means that normal pleasures provide even less reward than before, creating a vicious cycle where only the substance can penetrate the blunted reward system.
Recovery requires time for receptors to upregulate again, typically weeks to months of abstinence combined with metabolic support. This is the neurobiological basis of anhedonia during early recovery.
Reward Deficiency Syndrome
When dopamine function is chronically low—whether from genetic variants, nutrient deficiencies, toxin exposure, or chronic stress—the brain exists in a state of reward deficiency. Nothing feels good. Motivation disappears. Life feels flat and grey.
Substances that spike dopamine provide the only relief, creating rapid addiction vulnerability. This isn't psychological weakness; it's a starving system finally getting fed.
Signs You Have Dopamine Issues
- Anhedonia: Nothing brings pleasure; activities that used to be enjoyable feel empty
- Lack of motivation: Difficulty initiating tasks, procrastination, low drive
- Can't feel pleasure: Emotional flatness, numbness
- Attraction to stimulants: Coffee, nicotine, or harder stimulants feel necessary for functioning
- Difficulty focusing: Poor concentration, distractibility
- Low libido: Reduced sexual interest and pleasure
If these symptoms dominate your experience, dopamine dysfunction is likely a primary driver of addiction vulnerability.
Glutamate-GABA Imbalance
Glutamate is the primary excitatory neurotransmitter in the brain, driving neural activation and arousal. GABA (gamma-aminobutyric acid) is the primary inhibitory neurotransmitter, promoting calmness and relaxation. The balance between these two determines your baseline level of nervous system activation.
The Conversion Process
GABA is synthesized directly from glutamate via the enzyme glutamate decarboxylase (GAD). This enzyme has an absolute requirement for pyridoxal-5-phosphate (P5P), the active form of vitamin B6.
This single enzymatic step is where many people's systems break down. Standard B6 (pyridoxine) must be converted to P5P through a process requiring riboflavin (B2) and zinc. Research suggests up to 30% of people have genetic variants or enzyme deficiencies that impair this conversion, leaving them functionally deficient in P5P even with adequate dietary B6.
Without sufficient P5P, glutamate accumulates while GABA remains depleted. The result is a brain stuck in overdrive: anxious, racing thoughts, insomnia, hypervigilance, and an inability to relax.
Alcohol as Glutamate-GABA Medication
Alcohol's primary mechanism is enhancing GABA receptor function while blocking NMDA glutamate receptors. For someone with chronically high glutamate and low GABA, alcohol provides immediate relief—often the first time they've felt calm in years.
This is why people with glutamate-GABA imbalance often say, "Alcohol made me feel normal for the first time." They're not seeking intoxication; they're seeking nervous system balance they can't achieve biochemically.
Magnesium's Critical Role
Magnesium acts as a natural NMDA receptor blocker, preventing excessive glutamate signaling. It also serves as a cofactor for GAD and is required for GABA receptor function. Magnesium deficiency—extremely common due to depleted soil, processed foods, and stress—directly creates glutamate-GABA imbalance.
Zinc Modulation
Zinc modulates both glutamate and GABA receptors, generally inhibiting excessive glutamate activity. Zinc deficiency (common in alcoholics due to depletion and malabsorption) removes this protective modulation, increasing excitotoxicity.
Astrocyte Glutamate Clearance
After glutamate is released at synapses, astrocytes (supportive brain cells) must actively clear it from the extracellular space to prevent excitotoxicity. This clearance process requires ATP—energy from mitochondria.
When mitochondrial function is impaired (see next section), glutamate clearance becomes sluggish, leading to accumulation and chronic excitatory signaling. This creates a link between energy metabolism and neurotransmitter balance.
Signs You Have Glutamate-GABA Imbalance
- Chronic anxiety: Persistent worry, nervous energy, feeling "wired"
- Insomnia: Difficulty falling asleep, racing thoughts at night
- Can't relax: Physical tension, inability to "turn off"
- Hypervigilance: Constant scanning for threats, easily startled
- Alcohol provides profound relief: First drink feels like coming home
- Sensitivity to stimulants: Coffee makes you anxious and jittery
- Muscle tension: Tight shoulders, jaw clenching, headaches
If these symptoms dominate, glutamate-GABA imbalance is likely a primary driver, and addressing P5P, magnesium, and glutamate reduction should be priorities.
Mitochondrial Energy Crisis
Mitochondria are the energy factories in every cell, producing ATP through a complex series of reactions called the electron transport chain. Neurotransmitter synthesis, receptor function, and cellular repair all require enormous amounts of ATP.
When mitochondrial function is impaired, the brain operates in an energy-starved state. Neurotransmitter production decreases because there isn't enough ATP to fuel synthesis pathways. Receptor sensitivity changes as cells try to compensate for reduced signaling. Detoxification pathways slow because they're energy-expensive.
Nutrient Requirements
The electron transport chain requires specific nutrients:
- Coenzyme Q10 (CoQ10): Electron carrier in the chain; production decreases with age and statin use
- Iron: Component of cytochromes in complexes III and IV
- B vitamins: B1, B2, B3, B5 all serve as cofactors for energy metabolism
- Magnesium: Required for ATP synthesis and utilization
- L-carnitine: Transports fatty acids into mitochondria for fuel
Deficiency in any of these creates bottlenecks in ATP production.
Oxidative Stress and Mitochondrial Damage
Mitochondria are vulnerable to oxidative stress from:
- Toxins: Heavy metals, pesticides, air pollution
- Inflammation: Cytokines increase reactive oxygen species (ROS)
- Chronic stress: Cortisol increases mitochondrial ROS production
- Substance use: Alcohol and drugs directly damage mitochondria
As ROS accumulates, it damages mitochondrial DNA and membranes, reducing energy production capacity. This creates a vicious cycle: impaired mitochondria produce more ROS while having less capacity to neutralize it.
The Vicious Cycle
Energy crisis → reduced neurotransmitter synthesis → reward deficiency → increased substance use → more mitochondrial damage → worse energy crisis.
Additionally, impaired ATP production means:
- Less detoxification: Phase II liver detox requires ATP, leading to toxin accumulation
- Poor glutamate clearance: Astrocytes can't clear excess glutamate, increasing excitotoxicity
- Reduced GABA synthesis: GAD enzyme requires ATP for optimal function
- Impaired receptor sensitivity: Cells can't maintain proper receptor density
Energy-Starved Reward Systems
When the brain's reward circuits are energy-starved, they become hypersensitive to any source of stimulation. Substances that artificially activate these pathways feel dramatically more rewarding than they would in a metabolically healthy brain.
This is why addressing mitochondrial function is foundational—without adequate ATP, neurotransmitter restoration protocols will have limited effectiveness.
Signs of Mitochondrial Dysfunction
- Chronic fatigue: Exhaustion that isn't relieved by sleep
- Brain fog: Difficulty thinking clearly, poor memory
- Everything feels harder: Simple tasks require enormous effort
- Poor exercise tolerance: Unusual fatigue from mild activity
- Slow recovery: Taking days to recover from stress or exertion
- Multiple system dysfunction: When many symptoms exist simultaneously, suspect mitochondrial issues
If energy crisis dominates your symptom picture, mitochondrial support should be a primary focus.
Heavy Metal Toxicity
Heavy metals directly interfere with neurotransmitter synthesis and receptor function, creating addiction vulnerability. Unlike nutrient deficiencies that can be corrected in weeks, heavy metal toxicity often reflects decades of accumulation and requires months to years of careful detoxification.
Mercury and Alcoholism
Mercury has a specific affinity for sulfur-containing enzymes and interferes with multiple aspects of neurotransmitter metabolism. Research shows higher mercury levels in alcoholics compared to controls, and the mercury-alcohol connection is particularly strong (see Mercury and Alcoholism for detailed coverage).
Mercury specifically:
- Inhibits tyrosine hydroxylase (dopamine synthesis)
- Impairs GAD enzyme (GABA synthesis)
- Damages mitochondria
- Increases oxidative stress
- Creates alcohol cravings through direct neurochemical mechanisms
Lead and Impulsivity
Lead toxicity is associated with increased impulsivity, aggression, and poor executive function—all traits that increase addiction vulnerability. Lead accumulates in bones over a lifetime and can be released during periods of stress, pregnancy, or bone loss, creating delayed toxic effects.
Children exposed to lead have significantly higher rates of substance abuse in adulthood, demonstrating the long-term neurological impact.
Cadmium and Zinc Displacement
Cadmium, primarily from cigarette smoke and contaminated food, displaces zinc from binding sites. Since zinc is required for:
- Converting B6 to P5P
- Modulating glutamate receptors
- Supporting immune function
- DNA synthesis and repair
Cadmium toxicity creates downstream effects throughout neurotransmitter metabolism.
Accumulation and Transmission
Heavy metals accumulate over decades from:
- Dental amalgams: Mercury continuously releases vapor
- Fish consumption: Methylmercury in larger fish
- Occupational exposure: Mining, manufacturing, construction
- Environmental pollution: Coal-fired power plants, industrial areas
- Contaminated water: Lead pipes, well water
- Cigarette smoke: Cadmium and other metals
Critically, heavy metals can be transmitted generationally—from mother to fetus during pregnancy and through breast milk. Children born with higher toxic burdens start life with compromised neurological function.
Signs of Heavy Metal Toxicity
- Metallic taste: Persistent metallic taste in mouth
- Brain fog: Difficulty concentrating, memory problems
- Anxiety: Unexplained nervousness, panic
- Tremors: Hand tremors, muscle twitching
- Specific substance cravings: Particularly mercury-alcohol association
- Multiple chemical sensitivity: Reactions to perfumes, cleaning products
- Chronic inflammation: Elevated inflammatory markers without clear cause
Heavy metal testing (provoked urine tests via Doctor's Data or blood tests via Quicksilver Scientific) can identify specific toxic burdens and guide detoxification protocols.
Serotonin Depletion
Serotonin regulates mood, sleep, appetite, and impulse control. While often discussed as a brain chemical, 90% of serotonin is actually synthesized in the gut—making digestive health critical for mental health.
The Synthesis Pathway
Serotonin synthesis follows these steps:
- Tryptophan → 5-HTP: Catalyzed by tryptophan hydroxylase, requiring iron and BH4 (which needs folate, B2, B3, magnesium)
- 5-HTP → Serotonin: Catalyzed by aromatic amino acid decarboxylase, requiring P5P (active B6)
Notice that the second step is the same enzyme that converts L-DOPA to dopamine. This means serotonin and dopamine synthesis compete for the same enzyme, and both absolutely require P5P.
Tryptophan Competition
Tryptophan must cross the blood-brain barrier using the same transporter as other large amino acids (tyrosine, phenylalanine, leucine, isoleucine, valine). High-protein diets can reduce tryptophan entry into the brain by increasing competition.
Additionally, inflammation activates the kynurenine pathway, shunting tryptophan away from serotonin synthesis toward production of inflammatory compounds. This is a key mechanism by which chronic inflammation causes depression and addiction vulnerability.
Gut Dysfunction and Serotonin
Since 90% of serotonin is made in the gut by enterochromaffin cells, gut dysfunction directly impairs serotonin production:
- Dysbiosis: Imbalanced gut bacteria produce less serotonin
- Inflammation: Intestinal inflammation impairs enterochromaffin cells
- Nutrient malabsorption: Poor absorption of cofactors (iron, B6, folate)
- Leaky gut: Allows inflammatory compounds into bloodstream
People with IBS, SIBO, or other digestive issues often have concurrent mood disorders—this isn't coincidental but reflects shared serotonin dysfunction.
Serotonin and Addiction
Low serotonin manifests as:
- Depression and hopelessness
- Poor sleep quality
- Carbohydrate cravings (carbs temporarily boost serotonin)
- Mood instability
- Aggressive or impulsive behavior
Substances that boost serotonin (MDMA, some psychedelics) or those that indirectly affect it (alcohol through stress reduction) become highly reinforcing for people with serotonin depletion.
Signs of Serotonin Depletion
- Depression: Persistent low mood, hopelessness
- Poor sleep: Difficulty falling asleep, non-restorative sleep (serotonin converts to melatonin)
- Carb cravings: Strong desire for bread, pasta, sweets
- Mood instability: Rapid mood swings, irritability
- Aggressive impulses: Difficulty controlling anger
- Digestive issues: IBS, constipation, or diarrhea
- Seasonal affective disorder: Worse mood in winter months
Addressing gut health, ensuring adequate tryptophan intake, and providing synthesis cofactors are critical for restoring serotonin function.
Chronic Neuroinflammation
Inflammation in the brain disrupts virtually every aspect of neurotransmitter metabolism, creating a hostile environment for normal neurological function. While acute inflammation is protective, chronic neuroinflammation is destructive.
Sources of Neuroinflammation
- Gut dysbiosis: LPS (lipopolysaccharide) from gram-negative bacteria crosses leaky gut, triggering systemic inflammation
- Food sensitivities: Gluten, dairy, and other reactive foods create immune activation
- Chronic infections: Persistent viral, bacterial, or parasitic infections
- Toxic burden: Heavy metals, pesticides, mold toxins activate immune system
- Chronic stress: Cortisol initially suppresses inflammation but eventually causes immune dysfunction
- Substance use: Alcohol and drugs directly trigger inflammatory cascades
Inflammatory Cytokines and Neurotransmitters
Pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) directly interfere with neurotransmitter metabolism:
- Reduce dopamine synthesis: Cytokines inhibit tyrosine hydroxylase
- Increase glutamate: Inflammation impairs glutamate reuptake and clearance
- Decrease GABA: Inflammation reduces GAD activity
- Shunt tryptophan: Activate kynurenine pathway, reducing serotonin synthesis
- Damage mitochondria: Increase oxidative stress and reduce ATP production
This creates a state where excitatory signaling increases while inhibitory signaling and reward function decrease—precisely the neurochemical profile that drives addiction.
Microglial Activation
Microglia are the brain's immune cells. In healthy brains, they perform surveillance and cleanup. During chronic inflammation, they become activated and release inflammatory compounds that damage neurons, reduce neuroplasticity, and impair neurotransmitter function.
Activated microglia can persist for months to years even after the initial inflammatory trigger is removed, creating persistent neuroinflammation that resists treatment.
Blood-Brain Barrier Permeability
Chronic inflammation increases blood-brain barrier permeability, allowing inflammatory compounds, toxins, and pathogens that normally would be excluded to enter the brain. This creates a vicious cycle where systemic inflammation becomes neuroinflammation.
The Addiction-Inflammation Cycle
Substance use → increased inflammation → neurotransmitter dysfunction → increased cravings → more substance use → more inflammation.
Alcohol, in particular, increases gut permeability (leaky gut), allowing bacterial endotoxins into the bloodstream, triggering systemic inflammation that reaches the brain. This is one mechanism by which alcohol consumption perpetuates itself.
Signs of Chronic Neuroinflammation
- General malaise: Feeling unwell without specific symptoms
- Multiple sensitivities: Reacting to foods, chemicals, environmental factors
- Brain fog: Cognitive dysfunction, difficulty concentrating
- Immune dysfunction: Frequent infections or autoimmune conditions
- Poor stress tolerance: Small stressors feel overwhelming
- Elevated inflammatory markers: High CRP, IL-6, or other markers on testing
Addressing inflammation sources (gut healing, food elimination, toxin reduction, stress management) is critical for lasting recovery.
How Systems Interact and Compound
The systems described above don't fail independently—they form an interconnected web where dysfunction in one area cascades into others, creating compounding vulnerability.
Toxins → Inflammation → Neurotransmitter Dysfunction
Heavy metals trigger immune activation, creating chronic inflammation that disrupts neurotransmitter synthesis. Mercury specifically inhibits enzymes while also increasing inflammatory cytokines, creating a double mechanism of neurological damage.
Inflammation → Mitochondrial Damage → Energy Crisis
Inflammatory cytokines increase mitochondrial reactive oxygen species production while impairing antioxidant defenses. Damaged mitochondria produce less ATP, reducing capacity for neurotransmitter synthesis, detoxification, and cellular repair.
Energy Crisis → Impaired Detox → Toxin Accumulation
Phase II liver detoxification (conjugation reactions) requires ATP and nutrients (glutathione, sulfur, glycine). When mitochondria are impaired, detoxification slows, allowing toxins to accumulate, creating more oxidative stress and further mitochondrial damage.
Gut Dysfunction → Serotonin Depletion → Stress → Gut Dysfunction
Poor gut health reduces serotonin synthesis, contributing to depression and anxiety. This increases stress hormones, which further damage gut lining, worsen dysbiosis, and reduce serotonin production even more.
The Compounding Effect
When multiple systems are simultaneously impaired, they create a self-reinforcing cycle where each dysfunction makes the others worse. This is why:
- Single-nutrient approaches often fail (addressing one bottleneck while others persist)
- Symptom-only treatment provides temporary relief at best
- Comprehensive metabolic restoration is necessary for lasting recovery
Understanding these interactions allows you to identify which system failures are primary (causing others) versus secondary (resulting from others) in your specific case.
Individual Assessment Framework
Determining which systems are most compromised in your case allows targeted intervention rather than generic protocols. Use the following framework to assess your specific pattern.
Symptom Questionnaire
Rate each symptom cluster on a scale of 0-10 (0 = no symptoms, 10 = severe/constant):
Dopamine Dysfunction Score:
- Anhedonia, lack of pleasure
- Low motivation, procrastination
- Difficulty focusing
- Attraction to stimulants
- Low libido
Glutamate-GABA Imbalance Score:
- Chronic anxiety
- Insomnia, racing thoughts
- Can't relax
- Alcohol provides profound relief
- Muscle tension
Mitochondrial Dysfunction Score:
- Chronic fatigue
- Brain fog
- Everything feels harder
- Poor exercise tolerance
- Slow recovery
Heavy Metal Toxicity Score:
- Metallic taste
- Unexplained anxiety
- Tremors
- Multiple chemical sensitivity
- History of amalgam fillings or fish consumption
Serotonin Depletion Score:
- Depression
- Poor sleep quality
- Carb cravings
- Mood instability
- Digestive issues
Neuroinflammation Score:
- General malaise
- Multiple sensitivities
- Immune dysfunction
- Food reactions
- Elevated inflammatory markers (if tested)
The system(s) with the highest scores are likely your primary drivers of addiction vulnerability.
Testing Options
While symptoms provide valuable information, testing can confirm specific deficiencies and guide targeted treatment:
Neurotransmitter Testing:
- Urinary neurotransmitter panels (limitations: questionable correlation with brain levels)
- Better used for tracking changes over time than absolute diagnosis
Nutrient Testing:
- SpectraCell Micronutrient Test: Measures functional nutrient status in white blood cells
- NutrEval (Genova): Comprehensive nutrient assessment with organic acids
- Iron panel: Serum iron, ferritin, TIBC, transferrin saturation
- Magnesium RBC: More accurate than serum magnesium
Heavy Metal Testing:
- Doctor's Data Urine Toxic Metals: Provoked test using chelating agent
- Quicksilver Scientific Blood Metals: Distinguishes methylmercury from inorganic
- Hair mineral analysis: Reflects longer-term exposure (interpretation complex)
Gut Microbiome:
- GI-MAP (Diagnostic Solutions): Comprehensive stool test for pathogens, commensals, inflammation
- SIBO breath test: If small intestinal bacterial overgrowth suspected
Inflammation Markers:
- High-sensitivity CRP: General inflammation marker
- Cytokine panels: IL-6, IL-1β, TNF-α (specialty labs)
- Homocysteine: Methylation and inflammation marker
Mitochondrial Function:
- Organic Acids Test (Great Plains or Genova): Metabolic markers indicating mitochondrial efficiency
- CoQ10 levels: Direct measurement of key mitochondrial nutrient
Genetic Testing:
- COMT, MTHFR, GAD1, MAO variants: Inform neurotransmitter metabolism capacity
- 23andMe raw data can be uploaded to services like StrateGene or Genetic Genie for interpretation
Determining Primary vs. Secondary Issues
After assessing symptoms and ideally obtaining testing:
Primary issues are those that:
- Have the highest symptom scores
- Show significant abnormalities on testing
- Have clear causal mechanisms for other symptoms
- Appeared earliest in your health history
Secondary issues are those that:
- Result from primary issues
- Improve when primary issues are addressed
- Have less severe symptoms
- Appeared later in timeline
Example: If heavy metal testing shows high mercury, neuroinflammation markers are elevated, and mitochondrial function is impaired—mercury toxicity might be primary, with inflammation and energy crisis as secondary consequences. Addressing mercury detoxification would then be the priority.
Personalized Protocol Design
Once you've identified which systems are most compromised, you can design a targeted restoration protocol.
The Foundation (Everyone)
Regardless of which systems are primary, start with foundational support:
- Tier 1 Protocol (from main addiction article):
- Multivitamin with methylated B vitamins
- Magnesium glycinate 400-600mg
- Omega-3 fatty acids 2-3g EPA/DHA
- Vitamin D3 to achieve 50-70 ng/mL
- Probiotic for gut support
This addresses widespread deficiencies and supports all systems simultaneously.
Add Targeted Support Based on Assessment
If Dopamine Dysfunction is Primary:
- L-tyrosine: 500-1500mg morning and midday
- Iron (if deficient): Ferrous bisglycinate 25-50mg
- P5P (active B6): 50-100mg
- Methylfolate: 1-5mg (for BH4 synthesis)
- Copper (if deficient): 2-4mg
- Consider: Mucuna pruriens (natural L-DOPA source)
If Glutamate-GABA Imbalance is Primary:
- P5P (active B6): 100-200mg (critical for GAD enzyme)
- Magnesium: Increase to 600-800mg, divided doses
- Taurine: 1-3g (inhibitory neurotransmitter support)
- L-theanine: 200-400mg (promotes GABA, reduces glutamate)
- Glycine: 3-5g before bed (inhibitory, improves sleep)
- Consider: GABA supplementation (limited BBB penetration but some benefit)
If Mitochondrial Dysfunction is Primary:
- Coenzyme Q10: 200-400mg (ubiquinol form)
- L-carnitine: 1-2g
- Alpha-lipoic acid: 300-600mg (antioxidant, mitochondrial support)
- D-ribose: 5-15g (ATP precursor)
- Creatine: 5g (energy buffer)
- B-complex: High-dose B vitamins for electron transport chain
If Heavy Metal Toxicity is Primary:
- Support detox pathways FIRST (glutathione, NAC, selenium, molybdenum)
- Ensure adequate mineral status (zinc, magnesium, selenium)
- Binders: Chlorella, modified citrus pectin
- Then consider chelation: DMSA, DMPS, or EDTA under practitioner guidance
- Timeline: Months to years of gentle detoxification
If Serotonin Depletion is Primary:
- Heal gut first: Remove reactive foods, address dysbiosis/SIBO
- L-tryptophan: 500-2000mg evening or 5-HTP: 50-200mg
- Ensure cofactors: P5P, iron, methylfolate
- Anti-inflammatory diet to reduce kynurenine pathway
- Probiotic strains that support serotonin synthesis
If Neuroinflammation is Primary:
- Identify and remove inflammatory triggers (food sensitivities, gut infections, toxins)
- Heal gut barrier: L-glutamine, zinc carnosine, aloe
- Anti-inflammatory nutrients: Curcumin, omega-3s (high dose), resveratrol
- Support blood-brain barrier: Vitamin D, omega-3s
- Consider: Low-dose naltrexone (LDN) for microglial modulation
Example Protocols
Example 1: Dopamine-Primary Pattern
Sarah has severe anhedonia, low motivation, and attraction to stimulants. She has COMT Val/Val (fast breakdown) and low ferritin (iron storage).
Protocol:
- Foundation: Multivitamin, magnesium, omega-3, vitamin D
- L-tyrosine: 1000mg twice daily
- Iron bisglycinate: 25mg daily with vitamin C
- P5P: 50mg daily
- Methylfolate: 1mg daily
- Monitor energy and mood; adjust dosing after 4 weeks
Example 2: Glutamate-Primary Pattern
James has severe anxiety, insomnia, and racing thoughts. Alcohol provides immediate relief. He has always been "high-strung."
Protocol:
- Foundation: Multivitamin, magnesium, omega-3, vitamin D
- P5P: 150mg divided doses
- Magnesium glycinate: 200mg three times daily
- Taurine: 2g daily
- L-theanine: 200mg morning and evening
- Glycine: 5g before bed
- Remove caffeine entirely
Example 3: Gut-Primary Pattern
Lisa has depression, carb cravings, and IBS. She's had digestive issues for years before mood problems began.
Protocol:
- Phase 1 (8 weeks): Heal gut
- Eliminate gluten, dairy, processed foods
- Treat SIBO (if positive breath test)
- L-glutamine, zinc carnosine, probiotics
- Phase 2: Add neurotransmitter support
- L-tryptophan: 1000mg evening
- Continue gut support
- P5P, iron (if deficient)
Example 4: Toxin-Primary Pattern
Mark has high mercury levels, multiple chemical sensitivity, and anxiety. He has 8 amalgam fillings and ate tuna daily for years.
Protocol:
- Phase 1 (3 months): Support detox pathways
- NAC: 1200mg daily
- Selenium: 200mcg daily
- Glutathione support (liposomal or precursors)
- Ensure adequate zinc, magnesium
- Remove amalgams safely (biological dentist)
- Phase 2: Gentle chelation
- DMSA or ALA under practitioner guidance
- Continue binders (chlorella)
- Throughout: Support neurotransmitter systems to manage symptoms
Monitoring and Adjustment
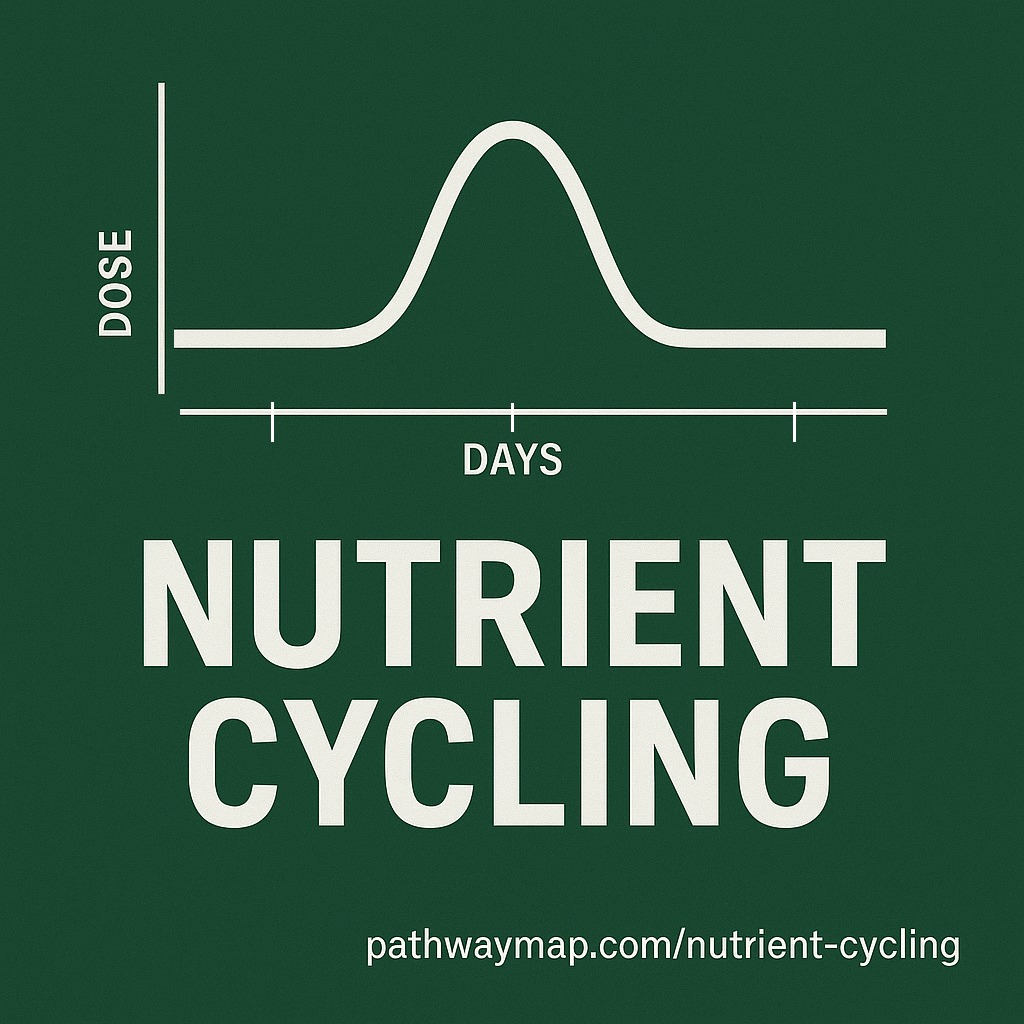
- Give time: Nutrient repletion takes weeks; receptor upregulation takes months
- Track symptoms: Use symptom scores weekly to assess response
- Adjust dosing: Increase if no response after 4 weeks; decrease if side effects
- Retest: Consider retesting key markers (nutrients, inflammation) at 3-6 months
- Be patient: Metabolic restoration is gradual, not instant
Why One-Size-Fits-All Fails
Conventional addiction treatment largely ignores metabolic factors, focusing instead on behavioral change and social support.
What Conventional Treatment Misses
12-Step Programs (AA, NA):
- Provide valuable social support and accountability
- Address behavioral patterns and psychological factors
- Work for some people (particularly those with strong social support needs)
- Miss entirely: Biochemical dysfunction, nutrient deficiencies, toxin burdens
- Result: High relapse rates when metabolic factors remain unaddressed
Medication-Assisted Treatment:
- Naltrexone: Blocks opioid receptors, reducing alcohol/opioid rewarding effects
- Buprenorphine: Partial opioid agonist, reduces withdrawal and cravings
- Addresses receptor level but not synthesis capacity
- Doesn't restore dopamine production, GABA synthesis, or mitochondrial function
- Result: Symptoms managed but underlying dysfunction persists
Psychotherapy:
- Cognitive-behavioral therapy addresses thought patterns
- Trauma therapy addresses psychological wounds
- Both valuable for recovery
- Don't address: Broken neurotransmitter synthesis, nutrient deficiencies, inflammation
- Result: Limited effectiveness when biochemistry is severely impaired
Individual Variation Requires Personalization
Why does AA work for one person but not another? Why does naltrexone help some and not others? Individual metabolic variation.
Person A: Primarily psychological and social factors driving addiction, relatively intact metabolic function. AA provides exactly what they need—social support and behavioral change.
Person B: Severe dopamine dysfunction from COMT variants, iron deficiency, and chronic stress. AA provides social support but doesn't address the metabolic crisis. Without dopamine restoration, behavioral changes feel impossible.
Person C: Mercury toxicity from amalgams creating GABA dysfunction and alcohol cravings. Naltrexone blocks opioid receptors but doesn't address mercury or GABA synthesis. Cravings persist.
One-size-fits-all fails because the biochemical patterns are dramatically different from person to person. Personalized metabolic assessment identifies the specific pattern and allows targeted intervention.
The Path Forward
Recovery from addiction through metabolic restoration follows a systematic path:
1. Identify Your Pattern
Use the symptom assessment to determine which systems are most compromised. Consider testing to confirm specific deficiencies or toxic burdens.
2. Address Foundations First
Regardless of your specific pattern, start with foundational support:
- Nutrient repletion (multivitamin, magnesium, omega-3s, vitamin D)
- Remove inflammatory foods
- Support gut health
- Manage stress
- Sleep optimization
These create a stable base for targeted interventions.
3. Add Targeted Support
Based on your primary dysfunction:
- Dopamine issues: Tyrosine, iron, cofactors
- Glutamate-GABA issues: P5P, magnesium, taurine
- Gut issues: Heal gut first, then neurotransmitter support
- Toxin issues: Support detox pathways, then gentle chelation
- Inflammation: Remove triggers, anti-inflammatory support
4. Monitor and Adjust
Track symptoms, energy, mood, and cravings. Adjust dosing and nutrients based on response. This is an iterative process requiring patience and observation.
5. Give Systems Time to Restore
Neurotransmitter synthesis improves within weeks as nutrients are repleted. Receptor upregulation takes months. Heavy metal detoxification takes months to years. Gut healing varies by severity.
Don't expect overnight transformation. Metabolic restoration is gradual, with improvements accumulating over time.
6. Cravings Reduce as Metabolism Normalizes
As dopamine synthesis improves, anhedonia lifts. As GABA production increases, anxiety decreases. As energy production normalizes, everything feels easier. As systems restore, the neurochemical drive toward substance use diminishes.
You're not "resisting temptation" through willpower—you're removing the metabolic dysfunction that created the craving in the first place.
7. Maintain Long-Term
Metabolic health requires ongoing maintenance:
- Continued nutrient supplementation (many people need lifelong support)
- Dietary quality
- Stress management
- Toxin avoidance
- Regular monitoring
This isn't a temporary fix but a shift to supporting your metabolic individuality.
Conclusion
Addiction emerges when multiple metabolic systems fail simultaneously, creating a neurochemical environment where substances become the only reliable source of reward, calm, or energy. Understanding which specific systems are broken in your case allows personalized restoration rather than generic treatment.
Your pattern is unique. Your genetics, toxic exposures, nutrient status, gut health, inflammation burden, and stress history create a specific constellation of metabolic dysfunction. Identifying this pattern and addressing it systematically offers a path forward that conventional treatment misses entirely.
The path is longer than "just stop using" but it's also more effective. As your dopamine synthesis improves, as your GABA production normalizes, as your mitochondria repair, as your toxic burden decreases—cravings diminish not through resistance but through metabolic restoration.
This is the difference between fighting against broken biochemistry and repairing it. One requires endless willpower; the other requires understanding your metabolic pattern and providing what your systems need to function again.