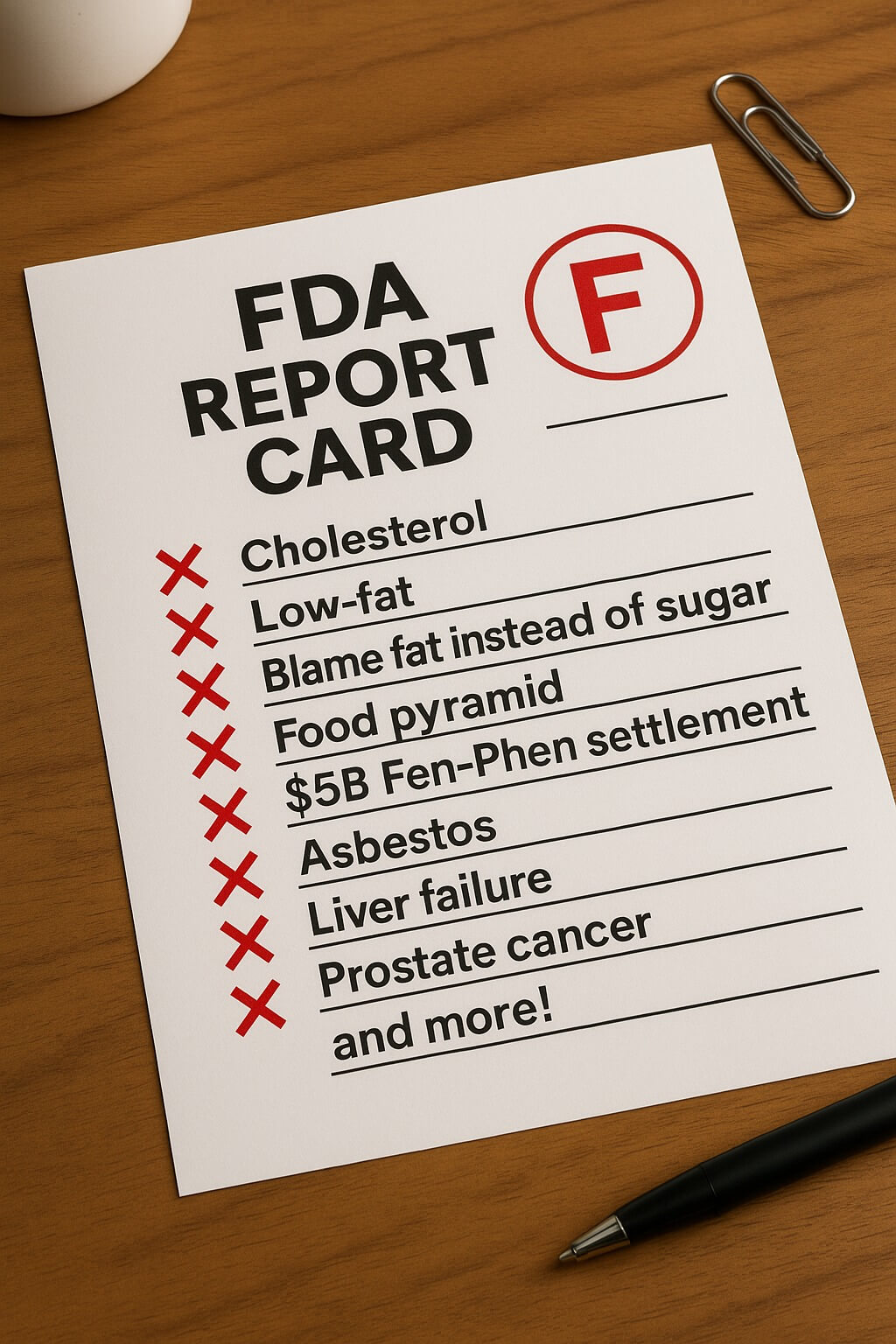
The FDA has reversed or significantly revised guidance on dozens of medications, foods, and health practices over the past 75 years, with some reversals taking over five decades to implement and causing hundreds of thousands of deaths or serious health impacts before corrections were made. These documented reversals demonstrate systematic patterns of premature recommendations, industry influence, and scientific overconfidence that continue to affect public health policy today, from the 54-year reversal on dietary cholesterol limits to the ongoing debates about COVID-19 guidance and chemical safety assessments.
This comprehensive analysis examines well-documented cases across seven categories of health recommendations, revealing that initial FDA approvals and public health guidance often prove inadequate when faced with longer-term studies and real-world evidence. The pattern suggests fundamental flaws in how health authorities evaluate evidence, respond to early warnings, and balance industry interests against public safety.
Dietary guidelines underwent complete reversals after decades of wrong advice
The most dramatic nutrition reversal occurred with dietary cholesterol, which health authorities restricted for 54 years before acknowledging the limits were unfounded. From 1961 to 2015, Americans were told to limit cholesterol to less than 300mg daily, causing egg consumption to drop 30% and creating billions in economic losses for farmers. The 2015 Dietary Guidelines Advisory Committee quietly removed this restriction after meta-analyses showed “no appreciable relationship between dietary cholesterol and serum cholesterol.” Similarly, the 35-year restriction on total fat consumption was abandoned in 2015 when research showed that limiting all fats, including beneficial ones, coincided with rising obesity rates as people replaced fats with refined carbohydrates.
The sugar industry’s role in shaping these flawed guidelines emerged through historical documents showing that the Sugar Research Foundation paid Harvard scientists $48,000 (in 2016 dollars) in the 1960s to downplay sugar’s role in heart disease while emphasizing fat’s dangers. This industry-funded research, published in the New England Journal of Medicine without disclosure, shaped dietary policy for decades. British researcher John Yudkin warned about sugar in the 1970s but was marginalized by the nutrition establishment, only to be vindicated decades later when his concerns about sugar became widely accepted.
The visual representation of nutrition advice also underwent major changes, with the 1992 Food Pyramid’s emphasis on 6-11 daily servings of grains now recognized as contributing to carbohydrate overconsumption. Harvard’s Walter Willett stated the original pyramid “contributes to overweight, poor health, and unnecessary early deaths.” The 2011 switch to MyPlate represented a complete abandonment of the pyramid concept after nearly 20 years of potentially harmful guidance.
Pharmaceutical approvals repeatedly failed with catastrophic consequences
The FDA’s drug approval process has produced numerous high-profile failures, with Vioxx representing the largest prescription drug withdrawal in history. Approved in 1999 and withdrawn in 2004, Vioxx caused an estimated 88,000 heart attacks and between 38,000 and 140,000 deaths in the United States alone. Internal documents revealed that Merck knew of cardiovascular risks as early as 1999 but argued that comparison drugs were cardioprotective rather than acknowledging Vioxx’s dangers. The New England Journal of Medicine later stated it was “hoodwinked” by Merck’s selective data presentation.
Fen-Phen’s withdrawal in 1997 after causing heart valve damage in 30% of long-term users demonstrated how drugs can gain widespread use without proper safety evaluation. Despite 18 million prescriptions written in 1996, the combination was never formally approved by the FDA. The disaster resulted in a $4.83 billion settlement and highlighted how off-label prescribing can circumvent safety reviews. Other major withdrawals included Baycol (52 deaths worldwide from muscle breakdown), Rezulin (63 deaths from liver failure), and numerous drugs that required black box warnings only after widespread harm occurred.
The accelerated approval pathway has become particularly problematic, with Aduhelm’s 2021 Alzheimer’s approval occurring despite a 10-0 advisory committee vote against it and three committee members resigning in protest. The drug was approved based on reducing amyloid plaques (a surrogate endpoint) without demonstrating cognitive improvement, then withdrawn in 2024 after failing to show clinical benefit. Similarly, Makena remained on the market for 12 years as the only FDA-approved drug for preventing preterm birth before being withdrawn in 2023 when confirmatory trials showed no benefit to newborns.
Medical procedures once considered standard care were abandoned after causing harm
The Women’s Health Initiative’s 2002 findings on hormone replacement therapy represent one of medicine’s most significant reversals. For over 40 years, at least 40% of postmenopausal women took HRT for chronic disease prevention, only to discover it increased risks of breast cancer, stroke, blood clots, and dementia. The estrogen-plus-progestin arm of the 27,347-woman study was halted early due to increased breast cancer risk, with HRT use dropping by almost 50% within months of the results’ publication.
Prostate cancer screening guidelines have reversed multiple times, with PSA testing going from routine in the 1990s to “not recommended” in 2012, then back to “individual decision” in 2017. Studies showed that over 10 years of frequent screening, false-positive rates exceeded 45%, leading to unnecessary biopsies and treatments that caused long-term urinary incontinence in 20% of men and erectile dysfunction in 67%.
Surgical practices also underwent major reversals. Episiotomy rates dropped from 63% of vaginal births in 1969 to 10.4% in 2018 after research showed the procedure actually caused worse tearing than natural childbirth. The Halsted radical mastectomy dominated breast cancer treatment for 80 years before studies in the 1970s-1980s proved that less invasive lumpectomy with radiation provided equivalent survival rates. Arthroscopic knee surgery for osteoarthritis, once performed over 650,000 times annually at $5,000 each, was found no better than placebo in 2002 trials, leading to a 47% reduction in procedures and saving $82-138 million annually.
Food additives deemed safe for decades were eventually banned
Trans fats underwent the most complete reversal in food additive history. Partially hydrogenated oils were classified as “Generally Recognized as Safe” (GRAS) in the 1960s and widely promoted as healthier alternatives to saturated fats. After 50+ years of widespread consumption, the FDA banned trans fats in 2018, but not before they contributed to an estimated 20,000+ coronary heart disease deaths annually. Denmark had banned trans fats 15 years earlier in 2003, demonstrating how the US regulatory system lagged behind international standards.
The artificial sweetener cyclamate was consumed by 175 million Americans in 250 food products before its 1970 ban due to bladder cancer in rats. Saccharin required cancer warning labels from 1977 to 2000 before being vindicated when the rat cancer mechanism was found not applicable to humans. Red Dye No. 3, approved in 1969 and linked to thyroid tumors, was bizarrely banned from cosmetics in 1990 but remained legal in food until January 2025—a 35-year regulatory inconsistency.
Brominated vegetable oil (BVO) remained in American beverages for over 50 years despite being banned in the UK (1970), EU (2008), and Japan (2010). Case reports documented patients losing the ability to walk after consuming 2-4 liters of BVO-containing soda daily. The FDA finally banned it in 2024, but major beverage companies had already voluntarily removed it after consumer petitions. The pattern of industry self-regulation preceding FDA action appeared repeatedly, with Olestra/Olean generating $400 million in sales before gastrointestinal side effects led to market abandonment rather than regulatory withdrawal.
Supplement recommendations promoted benefits that turned into dangers
The reversal on beta-carotene supplements represents one of the most dramatic supplement failures. Promoted throughout the 1980s for cancer prevention based on observational studies, two major trials in the 1990s found beta-carotene actually increased lung cancer risk by 18-28% in smokers. The CARET trial was terminated early due to a 17% increase in deaths, potentially causing hundreds of excess cancer deaths among participants alone.
Vitamin E’s trajectory from heart disease prevention miracle to potential harm took over a decade to unfold. The 1996 Cambridge Heart Antioxidant Study showed a 47% reduction in cardiac events, leading to widespread supplementation. But larger trials from 2000-2005 involving over 50,000 participants found no cardiovascular benefit, with meta-analyses suggesting increased mortality at high doses. The American Heart Association withdrew its recommendation in 2008, but millions had taken ineffective supplements for over a decade.
Calcium supplements, universally recommended for bone health, were found to potentially increase heart attack risk by 30% in some studies. The Women’s Health Initiative and other trials raised cardiovascular concerns that fundamentally changed how supplements are prescribed, with current guidelines emphasizing dietary sources over pills.
COVID-19 guidance changed repeatedly as the pandemic evolved
The mask guidance reversal damaged public trust more than perhaps any other COVID-19 policy change. In March 2020, the WHO and CDC actively discouraged public mask-wearing, claiming insufficient evidence and potential harm from improper use. By April 2020, both agencies reversed course, but the delay during the pandemic’s critical early months may have cost thousands of lives. Dr. Anthony Fauci later acknowledged the initial anti-mask stance was partly to preserve supplies for healthcare workers, not purely based on scientific evidence.
The obsession with surface cleaning created what critics called “hygiene theater,” with billions spent on sanitization while airborne transmission was downplayed. The CDC didn’t fully acknowledge airborne spread as the primary transmission route until May 2021, despite aerosol scientists like Linsey Marr warning about it from early 2020. MIT research showing respiratory droplets could travel 23-27 feet contradicted the six-foot social distancing rule, which Fauci admitted in 2024 congressional testimony “sort of just appeared” without supporting data.
Vaccine transmission prevention claims proved particularly problematic when breakthrough infections became common with the Delta variant in July 2021. Initial statements suggesting vaccines would stop transmission supported divisive “vaccinated vs. unvaccinated” policies, but Pfizer later acknowledged they never tested transmission prevention in initial trials. The gradual acknowledgment that vaccines primarily prevent severe disease rather than transmission fueled vaccine hesitancy when early promises didn’t materialize.
Environmental and chemical safety assessments took decades to acknowledge deadly risks
DDT’s transformation from Nobel Prize-winning “miracle pesticide” to banned environmental toxin took 30 years. Advertisements in the 1940s proclaimed “DDT Is Good for Me!” while the chemical pushed bald eagles and other species toward extinction. Rachel Carson’s “Silent Spring” in 1962 documented wildlife impacts, but the US didn’t ban DDT until 1972, after an estimated 30 years of environmental contamination and thousands of affected children globally.
Lead in gasoline represents perhaps the most devastating public health failure, with an estimated 824 million IQ points lost in the US alone and 151 million excess mental health disorders. Despite worker deaths and warnings from public health experts like Dr. Alice Hamilton in 1925, tetraethyl lead remained in gasoline until 1986. The final global elimination didn’t occur until 2021, nearly a century after the first warnings.
Asbestos, marketed as the “magic mineral” for fireproofing, still kills over 40,000 Americans annually from diseases caused by past exposure. First cases of asbestosis were documented in 1924, yet the US didn’t achieve a comprehensive ban until 2024—a full century later. Thalidomide caused over 10,000 children to be born with severe limb deformities in just four years of marketing before withdrawal in 1961, demonstrating how quickly inadequate testing can produce tragedy.
Patterns reveal systemic failures requiring fundamental reform
These reversals reveal consistent patterns: premature consensus based on weak evidence, industry influence on research and regulation, dismissal of early warning signs, and resistance to change even after contradictory evidence emerges. The average delay between initial safety concerns and regulatory action spans 10-20 years, during which millions suffer preventable harm. Financial settlements for drug withdrawals alone exceed $15 billion, yet companies typically admit no wrongdoing and often profit more during marketing than they pay in penalties.
The GRAS loophole allows companies to self-certify food additives as safe without FDA notification, creating a system where thousands of substances enter the food supply without oversight. International comparisons consistently show the US trailing other developed nations by 5-15 years in banning harmful substances, suggesting that regulatory capture and industry influence compromise the FDA’s protective mission. These documented failures demonstrate that protecting public health requires higher evidence standards before making population-wide recommendations, greater transparency about uncertainty and industry funding, regular reassessment of existing guidelines, and adoption of precautionary principles that prioritize safety over commercial interests.