The Coimbra Protocol: Metabolic Dependency Masquerading as Cure
The Coimbra Protocol represents one of alternative medicine’s most controversial autoimmune treatments, using vitamin D doses 10-75 times higher than established safety limits. After analyzing peer-reviewed research, clinical trials, and critical scientific perspectives, the evidence strongly indicates this protocol creates metabolic dependency through immune suppression rather than delivering genuine cures.
The protocol requires lifelong treatment, not temporary intervention
The most revealing finding comes directly from protocol advocates themselves. Dr. Cicero Coimbra and certified practitioners explicitly state that patients “will need to continue taking a high dose of vitamin D and other cofactors throughout their lives to stay in remission.” Despite treating over 30,000 patients since 2012, no published studies examine what happens when patients discontinue treatment. The recent VITAL extension study (2024) with 21,592 participants confirms that vitamin D’s protective effects against autoimmune diseases disappear within two years of stopping supplementation, requiring “continuous basis for long-term prevention.”
This lifelong requirement fundamentally contradicts claims of “curing” autoimmune diseases. A true cure would restore normal immune function permanently, not require indefinite pharmaceutical-level interventions. The protocol’s own practitioners acknowledge that while some dose reduction may be possible after 1-2 years, complete cessation leads to symptom return. This pattern clearly indicates symptom management through continuous suppression rather than disease resolution.
Clinical trials fail to support efficacy claims
While Dr. Coimbra claims a 95% success rate in suppressing multiple sclerosis activity, rigorous clinical trials paint a starkly different picture. The largest randomized controlled trials specifically testing high-dose vitamin D for MS have consistently failed to demonstrate significant clinical benefits.
The SOLAR trial (229 patients, 14,007 IU daily) failed to achieve its primary endpoint of “No Evidence of Disease Activity.” The VIDAMS trial (172 patients, 10,400 IU daily for 96 weeks) found no significant difference in relapse rates or disability progression compared to low-dose vitamin D. The EVIDIMS trial similarly showed no significant clinical or MRI outcome improvements. A 2024 meta-analysis of eight RCTs with approximately 1,000 MS patients concluded that “vitamin D3 supplementation shows no clinical benefit in MS over 24-month timeframes.”
The only published safety study specific to the Coimbra Protocol (Amon et al., 2022) examined 319 patients over 3.5 years but focused exclusively on safety parameters rather than efficacy outcomes. No randomized controlled trials exist validating the protocol’s extreme doses of 35,000-200,000 IU daily. The evidence supporting the protocol consists primarily of a single pilot study with 25 patients examining skin conditions, anecdotal reports, and testimonials rather than rigorous scientific validation.
Immunomodulation mechanisms reveal suppression, not restoration
The protocol’s biochemical mechanisms, while sophisticated, fundamentally involve immune suppression rather than tolerance restoration. At supraphysiological doses averaging 35,291 IU daily, vitamin D shifts the immune system from pro-inflammatory Th1/Th17 responses toward anti-inflammatory Th2 and regulatory T cell dominance. This represents a pharmacological intervention that continuously tilts immune balance rather than addressing why the immune system became dysregulated initially.
The protocol operates on the hypothesis of “acquired vitamin D resistance” in autoimmune patients, claiming genetic polymorphisms and environmental factors create a need for extreme doses. However, 75% of studied patients show permanent genetic variations in vitamin D metabolism genes (CYP2R1, CYP27B1), meaning any “resistance” cannot be cured but only compensated for indefinitely. The protocol achieves its effects through massive upregulation of vitamin D receptors, suppression of parathyroid hormone to the lower third of normal range, and fundamental alterations in calcium metabolism requiring strict dietary restrictions.
These mechanisms parallel conventional immunosuppressants – continuously dampening immune responses rather than correcting underlying dysfunction. The enhanced regulatory T cell function and suppressed Th17 responses revert upon discontinuation, confirming the effect is suppressive rather than restorative.
Safety concerns and institutional warnings underscore risks
Major medical organizations universally reject the protocol’s extreme dosing. The NIH sets the upper safe limit at 4,000 IU daily, while the Coimbra Protocol uses 35,000-200,000 IU – doses that can cause severe hypercalcemia, kidney stones, renal dysfunction, and cardiovascular calcification. The Cleveland Clinic warns that vitamin D toxicity can cause “kidney failure, abnormal heart rhythm, unsteady gait and confusion.”
The protocol requires permanent dietary calcium restriction below 500mg daily (eliminating dairy products), minimum 2.5 liters of daily fluid intake, and regular monitoring of calcium, PTH, and kidney function. A Swiss case report documented a patient developing hypercalcemia and renal insufficiency after seven months on 100,000 IU daily. The German safety study found 27 patients required temporary vitamin D cessation due to elevated calcium excretion.
No regulatory body – including the FDA, EMA, or other major health authorities – has approved this protocol. The Endocrine Society’s 2024 guidelines specifically recommend against routine high-dose vitamin D supplementation. The U.S. Preventive Services Task Force found insufficient evidence for vitamin D supplementation to prevent disease. Multiple sclerosis organizations, including Overcoming MS, warn there is “currently no published medical evidence” supporting the protocol and highlight “potential for serious complications.”
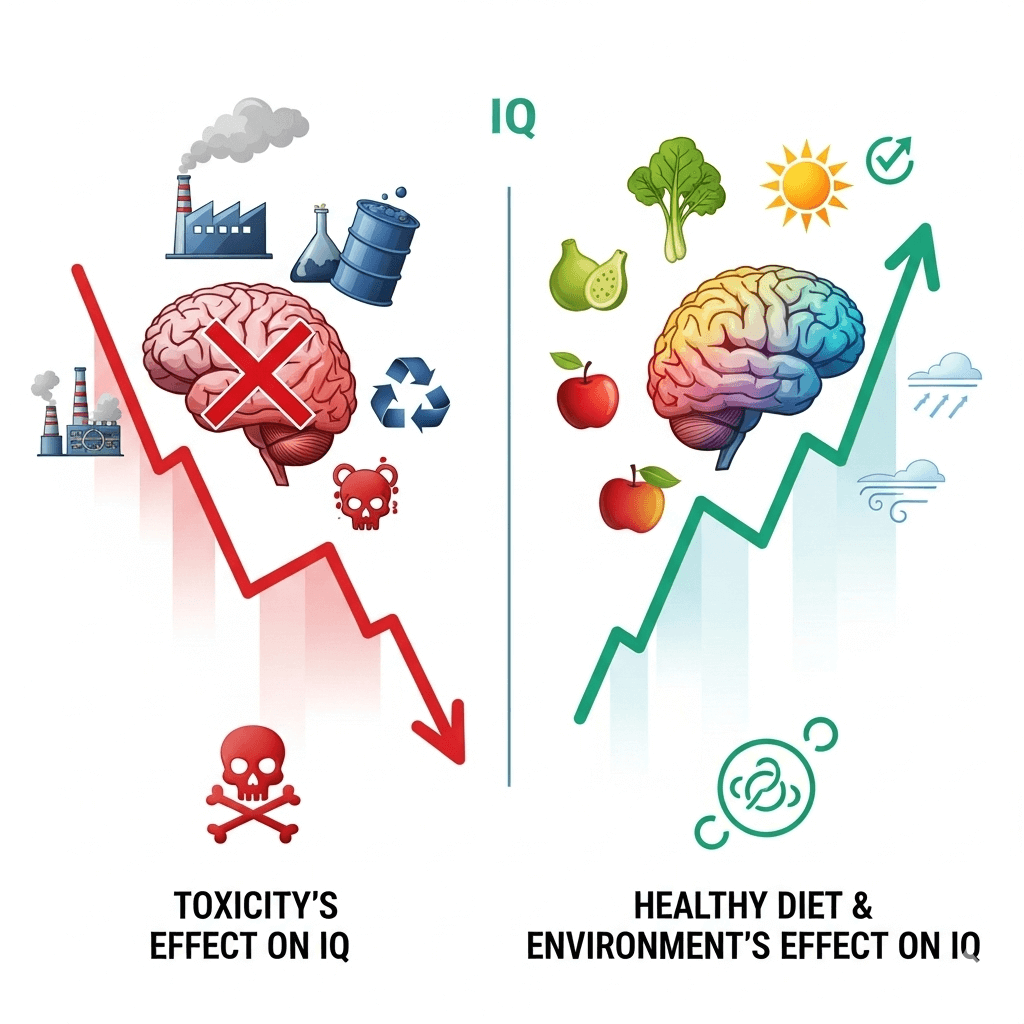
Root causes remain unaddressed while creating new dependencies
The protocol fails to address fundamental autoimmune triggers including environmental toxins, chronic stress, infectious agents, intestinal dysbiosis, or inflammatory dietary factors. Instead, it creates a new form of metabolic dependency where patients require lifelong supplementation at potentially dangerous doses to maintain symptom suppression.
Research on vitamin D withdrawal in other contexts consistently shows rapid return of inflammatory responses. Animal studies suggest high-dose vitamin D may cause “fulminant” autoimmune reactions when calcium levels rise after discontinuation. The protocol essentially trades one chronic condition for another – replacing active autoimmune disease with vitamin D dependency requiring permanent medical supervision.
Critically, no evidence exists for permanent immune system “reset” or tolerance restoration. The protocol doesn’t identify why specific individuals developed autoimmunity initially, nor does it remove causative factors. It represents downstream management rather than upstream intervention, similar to requiring insulin for diabetes without addressing insulin resistance causes.
Conclusion: Dependency marketed as cure lacks scientific support
The Coimbra Protocol exemplifies how alternative medicine can package chronic pharmaceutical dependency as natural healing. Despite over a decade of use and claims of treating 30,000 patients, the protocol lacks the fundamental hallmarks of a genuine cure: the ability to discontinue treatment while maintaining benefits, randomized controlled trials demonstrating efficacy, and evidence of addressing root disease causes rather than symptoms.
The protocol functions as a high-risk management strategy requiring lifelong adherence to potentially dangerous vitamin D doses, strict dietary restrictions, and continuous medical monitoring. While some patients may experience symptom improvement through immune suppression, they trade active disease for metabolic dependency with documented risks of hypercalcemia, renal dysfunction, and cardiovascular calcification.
Current scientific evidence suggests patients considering this approach should understand they are committing to permanent pharmacological intervention rather than achieving cure. The absence of discontinuation studies, failure of rigorous clinical trials to validate efficacy claims, and explicit statements from practitioners about lifelong treatment necessity all point to the same conclusion: the Coimbra Protocol represents sophisticated symptom suppression creating metabolic dependency, not the revolutionary cure its proponents claim.