Natural vitamin D recovery requires understanding how mercury damage, nutrient depletion, light exposure, and metabolic function interconnect as a complex biological system. Rather than simply supplementing isolated nutrients, successful restoration demands supporting the body’s natural processes through targeted nutrition, optimized sunlight exposure, and strategic lifestyle modifications.
Mercury Disrupts Vitamin D at the Molecular Level
Mercury’s devastating impact on vitamin D metabolism begins at the enzymatic level. The toxic metal binds irreversibly to sulfhydryl groups in cytochrome P450 enzymes, particularly CYP2R1 (25-hydroxylase) and CYP27B1 (1α-hydroxylase), permanently inactivating these critical hydroxylation steps. This disruption prevents the liver from converting vitamin D3 to 25(OH)D and blocks the kidney’s production of active 1,25(OH)2D. Mercury also damages mitochondrial membranes where these enzymes reside, reducing ATP production essential for vitamin D activation.
The nutritional balancing approach to mercury damage focuses not on chelation but on supporting damaged biochemical processes. Selenium forms inert mercury-selenium complexes with exceptionally high binding affinity (log K = 15-23), effectively neutralizing mercury’s toxic effects. L-selenomethionine at 200-400 mcg daily helps regenerate selenoproteins that mercury permanently inactivates. Zinc supplementation (15-30 mg daily) restores zinc finger proteins essential for vitamin D receptor function, while molybdenum (100-500 mcg) supports sulfur metabolism needed for glutathione synthesis. Magnesium becomes critically important as mercury toxicity increases cellular requirements while simultaneously depleting stores through oxidative stress.
Mercury’s interference extends beyond direct enzyme damage. It depletes glutathione by irreversibly binding to sulfhydryl groups, upregulates metallothionein synthesis (diverting sulfur compounds), and disrupts methylation pathways essential for vitamin D gene regulation. Supporting these systems requires methylfolate (400-800 mcg), methylcobalamin (1000-5000 mcg), and S-adenosylmethionine (400-800 mg daily) to maintain methylation capacity during recovery.
Fat Metabolism Determines Vitamin D Bioavailability
Vitamin D absorption fundamentally depends on proper fat digestion. As a fat-soluble vitamin, it requires bile acids from the liver and gallbladder to form micelles in the small intestine. Without adequate bile production, vitamin D absorption drops dramatically regardless of intake levels. Cholesterol serves as the direct precursor for vitamin D synthesis—7-dehydrocholesterol in skin converts to vitamin D3 upon UVB exposure. Traditional cultures consuming saturated animal fats showed optimal vitamin D status, while modern low-fat diets compromise this entire system.
The complete spectrum of vitamin D cofactors reveals intricate nutrient interdependencies. Magnesium is required for all vitamin D conversions, with 79% of US adults not meeting the RDA. Without magnesium, vitamin D remains inactive even at adequate blood levels. Vitamin K2 prevents the calcium paradox where bones weaken while arteries calcify—the MK-7 form at 90-360 mcg daily activates matrix GLA protein to direct calcium appropriately. Vitamin A partners with vitamin D at the nuclear receptor level, with both required for optimal gene transcription. Traditional cod liver oil provides the ideal A:D ratio nature intended.
Boron extends vitamin D’s biological half-life by up to 20% by inhibiting the 24-hydroxylase enzyme that degrades it. Just 3-10 mg daily from prunes, raisins, or leafy greens provides this often-overlooked mineral. Zinc enables proper vitamin D receptor DNA binding through zinc finger domains, while vitamin C at moderate doses (150 mg) enhances 1,25-dihydroxyvitamin D synthesis, though higher doses may actually inhibit activation.
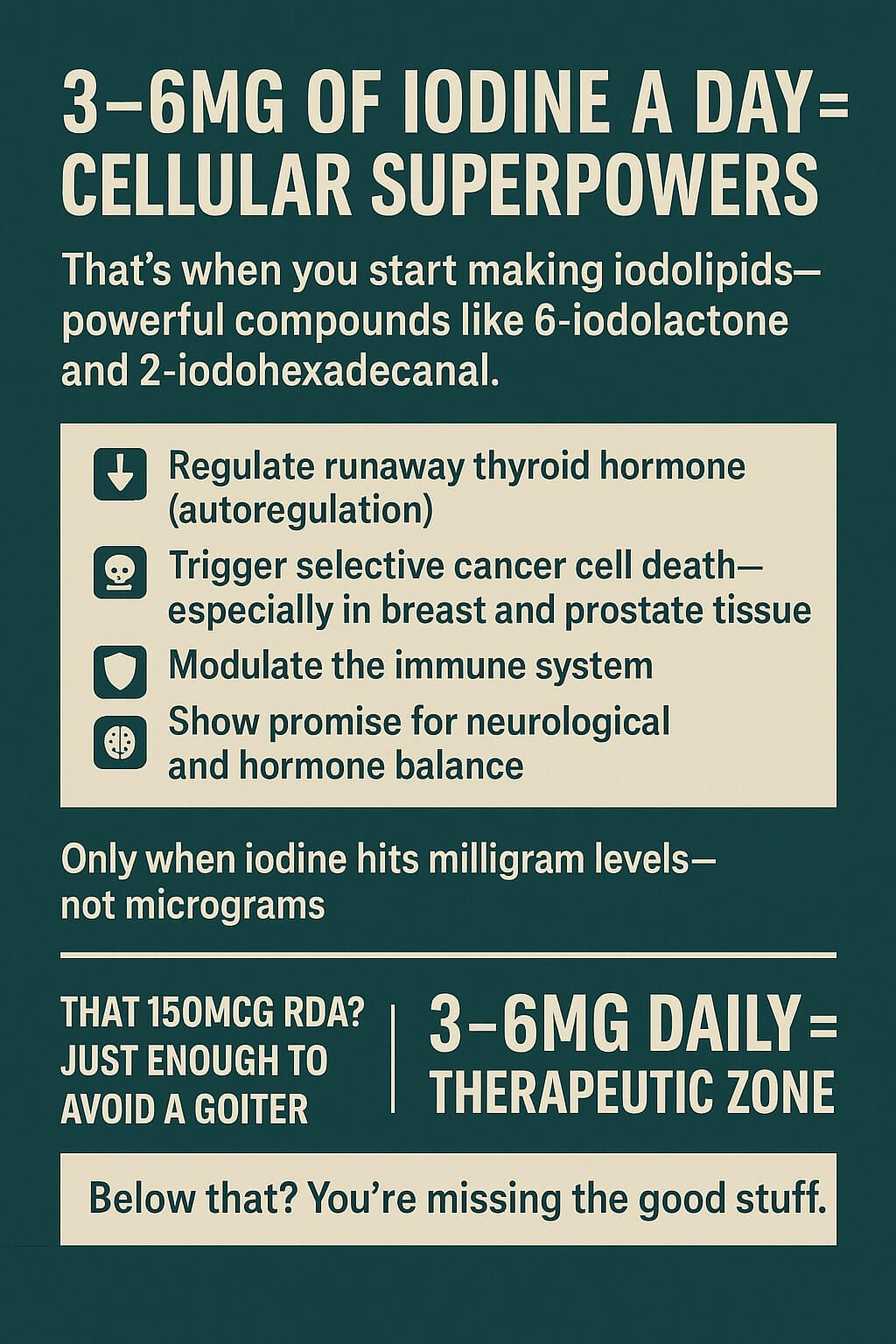
Iodine Deficiency Compounds Vitamin D Problems
Modern populations face widespread iodine deficiency from multiple factors: bromide displacement in processed foods, fluoride interference with utilization, depleted agricultural soils, and reduced seafood consumption. The thyroid-vitamin D connection runs deep—thyroid hormones regulate vitamin D metabolizing enzymes, while vitamin D deficiency strongly correlates with autoimmune thyroid conditions. Hypothyroidism impairs vitamin D metabolism, creating a vicious cycle of deficiency.
Safe iodine restoration requires starting with microgram doses (150-300 mcg daily), not the milligram doses often recommended. Kelp, dulse, and other seaweeds provide natural food sources. Adequate selenium and magnesium must be present before increasing iodine to prevent thyroid flares. Gradual increases over months allow the body to adapt without triggering autoimmune responses.
Sunlight Optimization Requires Understanding Solar Biology
Optimal vitamin D synthesis occurs between 10am and 2pm when the UV index exceeds 3. The shadow rule provides simple guidance: if your shadow is shorter than your height, UVB is available for vitamin D production. Duration varies by UV index—5-7 minutes at UV 14, 20-30 minutes at UV 3.5. Exposing 40% of body surface area proves more effective than longer exposure of smaller areas. Once skin produces its daily vitamin D quota, longer exposure provides no additional benefit.
Building solar tolerance requires systematic adaptation. Begin with 30+ minutes of sunrise exposure rich in protective infrared light, which prepares skin for later UV exposure. Start with 2-3 minutes per side in morning or late afternoon sun, gradually increasing by 1-2 minutes weekly. Never allow burning—stop at first sign of pinkness. The gradual spring progression from March 19th provides natural adaptation as UV levels increase seasonally.
Infrared and red light play crucial protective roles. Red light (630-700nm) and near-infrared (700-1000nm) provide protective effects against UV damage while enhancing cellular energy production for repair processes. Morning infrared exposure followed by midday UVB creates optimal conditions for vitamin D synthesis with minimal damage. Sunrise and sunset viewing entrains circadian rhythms through specialized melanopsin receptors, with 5-20 minutes of morning sun exposure critical for setting the biological clock.
Blue Light and EMF Disrupt Vitamin D Pathways
Artificial blue light after sunset completely suppresses melatonin production, disrupting circadian vitamin D receptor expression. Just 2 hours of 460nm blue light exposure eliminates melatonin, with peak disruption at 424nm wavelengths. Poor sleep from light pollution reduces vitamin D activation in kidneys by 25-40%. The solution requires blue-blocking glasses 2-3 hours before bed, red light for evening illumination, and complete darkness during sleep.
Non-native electromagnetic fields activate voltage-gated calcium channels, disrupting calcium homeostasis essential for vitamin D function. WiFi and cell phone radiation cause mitochondrial dysfunction, reducing energy available for vitamin D synthesis. Twenty-three studies confirm EMFs directly activate these channels, leading to oxidative stress through peroxynitrite pathways. Mitigation requires turning off WiFi routers at night, using airplane mode on devices, maintaining distance from electronics, and grounding outdoors daily for natural electromagnetic connection.
Northern Populations Developed Unique Adaptations
Traditional Arctic populations consumed massive amounts of seafood, with vitamin D concentrating up the ocean food chain. A single fish consumes 1.2% of its body weight in plankton daily; seals consume the equivalent of half a ton of plankton per pound of body weight. Killer whales get the equivalent of 5 tons of plankton per pound, explaining extremely high vitamin D concentrations in marine apex predators. Traditional sources included cod liver oil with vitamin D levels several times higher than ordinary oils, seal oil providing 200 calories daily in Inuit diets, and whole small fish like sardines and anchovies.
Cold exposure provides unexpected vitamin D support through brown fat activation and enhanced mitochondrial function. Traditional practices like Nordic winter swimming and Russian ice bathing may compensate for reduced sun exposure. Cold thermogenesis doubles metabolic rate during exposure, potentially supporting vitamin D utilization through improved mitochondrial biogenesis. Starting with 30 seconds to 1 minute in 50-59°F water, gradually building to 10-20 minutes, creates beneficial adaptive stress without overwhelming the system.
Fermentation techniques dramatically enhanced vitamin D bioavailability in traditional diets. Lacto-fermentation increased quinone content (including vitamin K2) by 700-1600% in cod liver oil. Traditional fermented fish products like nam-pla and fermented fish paste provided year-round vitamin D in preserved form. Even more remarkably, mammalian blood stores vitamin D primarily as calcidiol, which is 5 times more potent than unconverted D—traditional Maasai blood consumption could provide 8,000 IU per 2-cup serving.
Practical Implementation Follows Systematic Progression
Successful vitamin D restoration requires careful sequencing. First, test baseline 25(OH)D levels and address digestive health for proper absorption. Ensure adequate magnesium (400-800mg daily) before introducing vitamin D, as it’s required for all conversions. Rule out primary hyperparathyroidism, which contraindicates supplementation.
Begin vitamin D3 at 4,000-6,000 IU daily with cofactors, never in isolation. Add vitamin K2 (100-200mcg MK-7), vitamin A from cod liver oil, and maintain magnesium. Start gradual sun exposure with 10-15 minutes morning sun, increasing weekly toward midday exposure. Monitor 25(OH)D every 6-8 weeks initially, targeting 40-60 ng/mL for most people.
Building sun tolerance requires respecting adaptation capacity. Fair-skinned individuals need more gradual progression than darker skin types. Begin with morning sun when UVB is minimal, progress to late morning, then finally midday exposure. Combine with cold exposure protocols if geographically appropriate—both stresses create beneficial adaptations when applied gradually.
Common Mistakes Reveal System Interconnections
The most dangerous mistake involves high-dose vitamin D supplementation without cofactors. This depletes magnesium stores, creates functional vitamin A deficiency, and causes calcium dysregulation without K2. Isolated supplementation can increase cardiovascular disease risk by 31% through soft tissue calcification. Studies show 48-55% of Americans already consume inadequate magnesium, making depletion from vitamin D particularly problematic.
Ignoring bile and fat digestion prevents absorption regardless of intake. Conditions like gallbladder dysfunction, bile acid malabsorption, or inflammatory bowel diseases block vitamin D uptake entirely. Mercury and heavy metal burden creates a dual problem—vitamin D increases absorption of both essential minerals and toxic metals, while heavy metals block renal synthesis of active vitamin D.
Supplementing while maintaining poor light hygiene misses critical benefits. Sun exposure creates β-endorphins, nitric oxide, melatonin precursors, and other photoproducts beyond vitamin D. Eighty-seven genes show circadian patterns suppressed by artificial light exposure. Natural production provides tight regulatory control that supplementation cannot replicate.
Systems Biology Reveals the Complete Picture
Vitamin D restoration operates within interconnected biological networks where mercury damage affects nutrient absorption, which impairs vitamin D synthesis, while light exposure influences mineral metabolism and circadian rhythms affect nutrient utilization. Chronic stress elevates cortisol, interfering with vitamin D receptor function. Inflammation blocks receptors and reduces effectiveness. Insulin resistance creates bidirectional dysfunction with vitamin D deficiency.
Successful restoration requires addressing all system components simultaneously. Support bile production for absorption, reduce heavy metal burden gradually, optimize circadian rhythms through proper light exposure, address inflammation systemically, and restore insulin sensitivity. The timeline varies individually—energy and mood improvements often occur within 3-4 weeks, while complete optimization takes 3-6 months with proper cofactor support.
Conclusion
Natural vitamin D recovery demands far more than taking a supplement. It requires understanding and supporting the complex web of nutrients, light exposure, metabolic function, and environmental factors that enable vitamin D synthesis, activation, and utilization. Mercury damage must be addressed through targeted nutritional support of damaged pathways. Fat metabolism and bile production enable absorption. Nutrient cofactors prevent imbalances and toxicity. Sunlight exposure optimized for latitude and season provides benefits beyond vitamin D alone. Traditional dietary wisdom from northern populations offers time-tested solutions for low-sun environments.
Most critically, this systems biology approach recognizes that isolated interventions often fail or cause new problems. By supporting the body’s interconnected processes—from enzymatic function to circadian biology—we restore not just vitamin D levels but the entire biological system in which vitamin D operates. This comprehensive approach, respecting both traditional wisdom and modern biochemistry, provides the foundation for lasting vitamin D optimization and improved health outcomes.
Keep Going
Glyphosate is inhibiting “vitamin” D and its cofactors /sunlight-antibiotics