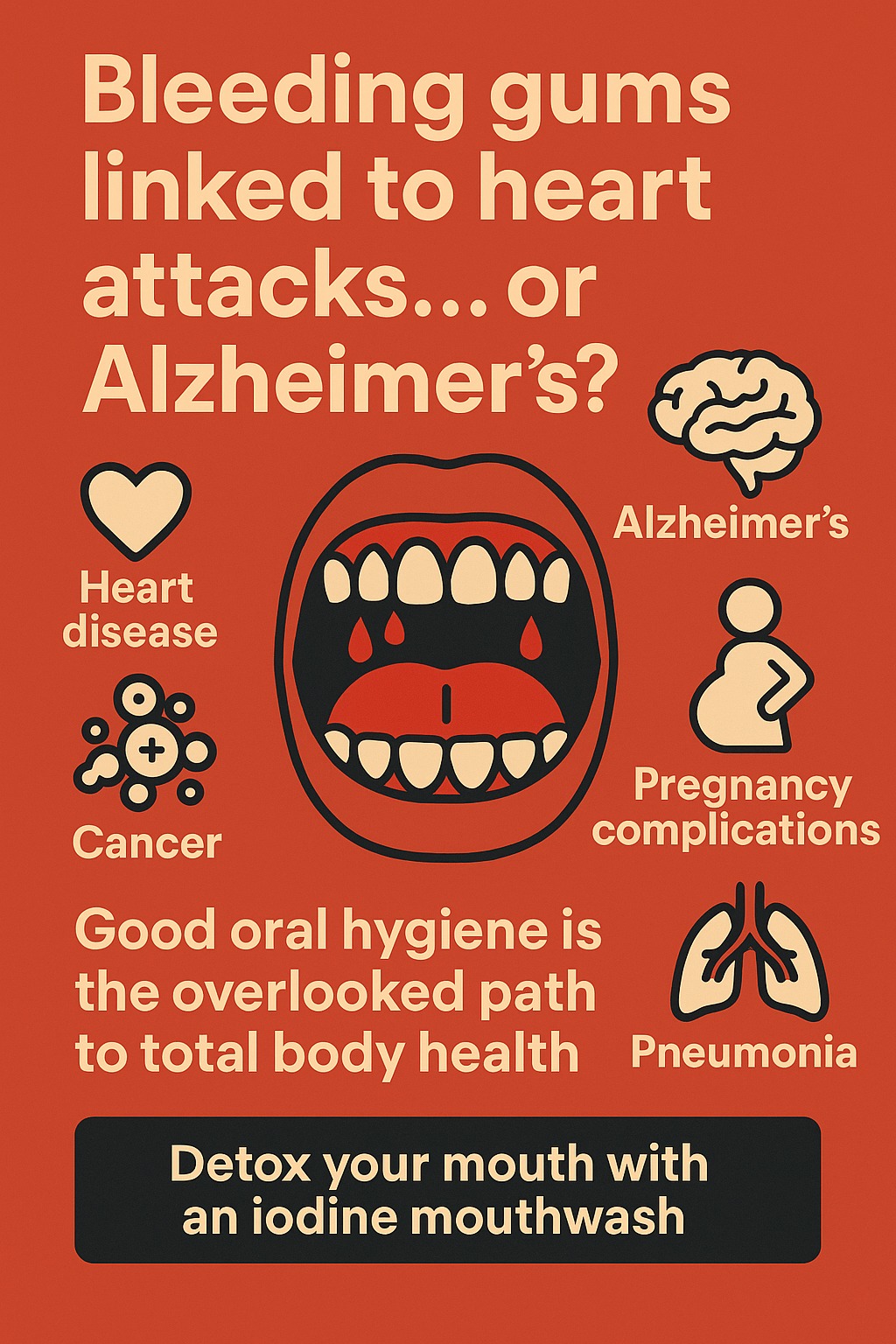
The mouth harbors the second most diverse microbial community in the human body, with over 700 bacterial species alongside fungi, viruses, and other microorganisms. This oral microbiome profoundly influences not just dental health but systemic conditions ranging from heart disease to Alzheimer’s, pregnancy complications, and cancer. Recent scientific breakthroughs have transformed our understanding from mere associations to mechanistic insights, revealing how oral bacteria travel through the body and trigger disease processes far from their origin.
The Complex Ecosystem Within Our Mouths
The oral microbiome consists of distinct microbial communities across different mouth regions, each with unique characteristics. The subgingival plaque beneath the gumline harbors the highest diversity with over 218 microbial genera, while the tongue dorsum serves as the primary reservoir feeding bacteria into saliva. In health, beneficial bacteria like Streptococcus mitis and Neisseria species dominate, performing crucial functions including nitrate reduction that helps regulate blood pressure and maintains oral pH balance.
The composition varies dramatically by location: the hard palate contains primarily Streptococcus species (44%), while subgingival areas harbor anaerobic bacteria like Actinomyces and Fusobacterium. This ecosystem remains relatively stable in healthy individuals but shifts dramatically during disease. Oral dysbiosis—the imbalance between beneficial and harmful bacteria—occurs when pathogenic species like Porphyromonas gingivalis overtake protective bacteria, triggering both local inflammation and systemic disease processes.
How Oral Bacteria Infiltrate the Body and Trigger Systemic Disease
Research reveals multiple pathways through which oral bacteria escape the mouth and affect distant organs. Daily activities like chewing and tooth brushing cause transient bacteremia, allowing bacteria to enter the bloodstream through inflamed gum tissue. The ulcerated epithelium in periodontitis creates a portal equivalent to a wound the size of the palm, providing continuous bacterial access to circulation.
Once in the bloodstream, oral pathogens employ sophisticated mechanisms to evade immune defenses and colonize distant sites. P. gingivalis produces gingipains—proteases that degrade antibodies and complement proteins while activating blood clotting cascades. These bacteria have been directly detected in atherosclerotic plaques (39-45% of samples), brain tissue of Alzheimer’s patients, and placental tissue in pregnancy complications. The oral-gut axis provides another route, with over 1000 mL of saliva swallowed daily carrying oral bacteria that can disrupt intestinal barriers and trigger inflammation.
Cardiovascular Disease: The Most Established Oral-Systemic Connection
The link between oral health and heart disease represents the most extensively studied oral-systemic connection. People with periodontal disease face 2-3 times higher risk of heart attack, stroke, or other serious cardiovascular events. Meta-analyses of over 20 studies confirm this association remains significant even after adjusting for shared risk factors like smoking and diabetes.
The mechanisms extend beyond simple bacterial presence. P. gingivalis appears in 45% of coronary atherosclerotic plaques, where its gingipains activate platelets and promote clot formation. Streptococcus mutans, found in 78% of cardiovascular thrombus tissues, directly accelerates plaque formation. These bacteria trigger systemic inflammation, with elevated C-reactive protein and IL-6 levels creating a pro-thrombotic state. The displacement of beneficial nitrate-reducing oral bacteria also impairs blood pressure regulation, as these species normally convert dietary nitrates to nitric oxide—a crucial vasodilator.
Alzheimer’s Disease: Breakthrough Discovery of Brain Invasion
Perhaps the most striking recent discovery involves P. gingivalis directly invading brain tissue in Alzheimer’s disease. A landmark 2019 study in Science Advances detected both the bacteria and its toxic gingipains in Alzheimer’s brain samples, with levels correlating with tau and amyloid pathology. Meta-analyses show 10.68-fold increased Alzheimer’s risk when oral bacteria are detected in the brain.
The bacteria cross the blood-brain barrier through multiple routes: gingipains degrade tight junction proteins, allowing direct passage; bacteria hide within immune cells that cross naturally; and chronic inflammation from oral infection compromises barrier integrity. Once in the brain, P. gingivalis triggers neuroinflammation, promotes amyloid-β production, and causes tau hyperphosphorylation—all hallmarks of Alzheimer’s pathology. Clinical trials of gingipain inhibitors are now underway as potential Alzheimer’s treatments.
Diabetes: A Destructive Bidirectional Relationship
The relationship between oral health and diabetes creates a vicious cycle. People with severe periodontitis show increased risk of developing type 2 diabetes, while diabetics experience more severe gum disease. High glucose levels in diabetic saliva feed pathogenic bacteria, while dehydration reduces protective saliva flow. The oral microbiome in diabetics shows decreased beneficial Actinobacteria and increased Firmicutes, with enhanced virulence factor production.
Remarkably, periodontal treatment improves diabetes control. Clinical trials demonstrate that professional gum disease treatment reduces HbA1c by 0.27-0.48%—comparable to adding a second diabetes medication. This improvement likely results from reduced systemic inflammation and decreased bacterial endotoxin levels that interfere with insulin signaling.
Pregnancy Complications Demand Urgent Attention
Oral bacteria significantly impact pregnancy outcomes, with periodontal disease linked to preterm birth, low birth weight, and preeclampsia. Clinical trials show periodontal treatment during pregnancy reduces preterm birth risk by 35% (OR 0.65) and low birth weight by 47% (OR 0.53), with the greatest benefit in high-risk populations.
P. gingivalis and Fusobacterium nucleatum appear at higher levels in women experiencing pregnancy complications. These bacteria travel through the bloodstream to colonize the placenta, where they trigger inflammatory cascades that can induce premature labor. The oral-to-gut translocation pathway also plays a role, with increased oral-origin bacteria detected in the gut microbiome of preterm birth patients.
Respiratory Infections: The Aspiration Connection
The mouth serves as a reservoir for respiratory pathogens, with dental plaque containing 100 million bacteria per cubic millimeter. Poor oral health increases pneumonia risk 2-9 fold, particularly concerning for elderly and hospitalized patients. Common respiratory pathogens including Streptococcus pneumoniae, Staphylococcus aureus, and Pseudomonas aeruginosa colonize dental plaque before aspiration into lungs.
Professional oral care in nursing homes and ICUs significantly reduces pneumonia incidence. The mechanism involves both direct aspiration of oral bacteria and the inflammatory burden from gum disease compromising respiratory defenses. COPD patients show particular vulnerability, with oral bacteria detected in lung samples during exacerbations.
Emerging Connections Spark New Research
Recent studies reveal surprising connections between oral health and additional conditions. In rheumatoid arthritis, P. gingivalis produces a unique enzyme that modifies proteins, creating autoantigens that trigger joint inflammation. This discovery explains why RA patients often experience gum disease years before joint symptoms and why periodontal treatment can reduce arthritis severity.
The oral microbiome also influences cancer risk. P. gingivalis activates cancer-promoting pathways in oral and pancreatic cancers, while F. nucleatum travels from mouth to colon where it promotes tumor growth and helps cancer cells evade immune detection. Salivary microbiome changes may even serve as early cancer biomarkers.
Testing Advances Enable Personalized Interventions
Commercial oral microbiome testing has evolved from research tool to clinical application. Next-generation sequencing platforms like Bristle Health analyze 700+ species from saliva samples for around $120, providing personalized recommendations. More targeted qPCR tests from companies like OralDNA Labs detect specific pathogens to guide treatment decisions.
Advanced shotgun metagenomics now reveals not just which bacteria are present but what they’re doing—identifying virulence genes, antibiotic resistance, and metabolic functions. Machine learning algorithms achieve 84.5% accuracy in predicting Parkinson’s disease from oral microbiome profiles alone, suggesting diagnostic potential for multiple conditions.
Novel Therapeutics Target the Microbiome
Treatment approaches have expanded beyond traditional antibiotics to microbiome-friendly interventions. Specific probiotic strains show clinical efficacy: Streptococcus salivarius K12 reduces pathogen levels and bad breath, while Lactobacillus reuteri improves gum inflammation markers. Multi-strain formulations outperform single strains, and synbiotic approaches combining probiotics with targeted prebiotics show particular promise.
Cutting-edge therapies include engineered bacteriophages that selectively eliminate pathogens while preserving beneficial bacteria. Over 3,000 antimicrobial peptides identified from natural sources offer antibiotic alternatives with lower resistance risk. CRISPR gene editing may soon enable precise microbiome modifications, converting disease-promoting communities to health-promoting ones.
Clinical Trials Pave the Path Forward
Major research initiatives are translating discoveries into practice. The NIH’s Functional Oral Microbiome program has shifted focus from cataloging bacteria to understanding their roles in health and disease. Clinical trials explore phage therapy for antibiotic-resistant oral infections, test antimicrobial peptides for gum disease, and investigate whether early microbiome interventions can prevent systemic diseases.
Several trials examine “replacement therapy”—introducing genetically modified beneficial bacteria to permanently colonize the mouth and crowd out pathogens. Others test personalized probiotic cocktails based on individual microbiome profiles. FDA approval of SER-109, an oral microbiome-derived therapeutic for C. difficile infections, validates the therapeutic potential of microbiome medicines.
Conclusion
The scientific evidence definitively establishes the oral microbiome as a critical determinant of systemic health. From the landmark discovery of P. gingivalis in Alzheimer’s brains to clinical trials showing periodontal treatment improves pregnancy outcomes and diabetes control, research has moved beyond correlation to demonstrate causation and mechanism. The oral cavity represents an accessible intervention point where simple preventive measures—regular professional cleanings, good oral hygiene, and microbiome-friendly approaches—can reduce risk for heart disease, dementia, adverse pregnancy outcomes, and more.
As testing becomes more sophisticated and treatments more targeted, oral microbiome management will likely become standard in personalized medicine. The mouth truly serves as a window to overall health, and maintaining its microbial balance emerges as one of the most impactful steps individuals can take for lifelong wellness. Healthcare must evolve to recognize that optimal oral health is not merely about preventing cavities—it’s about preventing many of our most devastating chronic diseases.
So how do we fix this?
Keep following me to learn how to support our cells the best we can.
Invest in this iodine mouthwash https://www.iotechinternational.com/product-page/iorinse-rtu-ready-to-use-mouth-rinse-soft-mint?ref=beginner which gets more iodine to our mouth than lugols could do even if we used enough to burn our skin with strong lugols