Mitochondrial dysfunction sits at the heart of chronic fatigue, brain fog, and countless modern health conditions, yet most treatments fail because they address symptoms in isolation rather than understanding the interconnected metabolic web that controls cellular energy production. Research reveals that successful mitochondrial restoration requires simultaneous optimization of circadian rhythm, digestive health, mineral balance, and multiple metabolic pathways – a level of complexity that fragmented medical approaches systematically miss, leaving patients stuck in treatment loops while the real solutions hide in plain sight.
The energy production machinery requires precise orchestration
Mitochondria operate like sophisticated biochemical factories where the Krebs cycle and electron transport chain transform nutrients into ATP through an intricate dance of enzymes and cofactors. Each step requires specific nutrients: thiamine for pyruvate dehydrogenase, riboflavin for electron transport complexes, iron for cytochromes, and magnesium for ATP synthesis itself. When even one cofactor becomes limiting, the entire energy production line slows down.
The α-ketoglutarate dehydrogenase complex serves as a particularly vulnerable bottleneck – this rate-limiting enzyme in the Krebs cycle requires five essential cofactors and is exquisitely sensitive to oxidative stress. When inflammation, toxins, or nutrient deficiencies impair this enzyme, downstream energy production collapses regardless of how many other supplements someone takes. This explains why comprehensive cofactor support often succeeds where single nutrients fail.
Modern research shows that cardiolipin, a unique phospholipid found only in mitochondrial membranes, stabilizes respiratory complexes and determines energy production efficiency. Without adequate phospholipids from proper fat digestion and bile flow, mitochondrial membranes become dysfunctional regardless of how many B-vitamins someone consumes. This membrane composition factor represents a critical missing piece in most mitochondrial support protocols.
Why people megadose thiamine: Bypassing metabolic roadblocks through saturation
The phenomenon of high-dose thiamine therapy (300-1800mg daily, versus the 1.2mg RDA) illuminates a crucial concept in metabolic medicine: functional deficiency. Pioneering researchers Dr. Derrick Lonsdale and Dr. Chandler Marrs discovered that many people have normal blood thiamine levels yet respond dramatically to megadoses because their thiamine-dependent enzymes have lost affinity for the cofactor due to oxidative damage, genetic variations, or chronic inflammation.
When the pyruvate dehydrogenase and α-ketoglutarate dehydrogenase complexes become damaged or inhibited, they require much higher thiamine concentrations to function normally. Megadosing works through mass action – saturating cells with enough thiamine pyrophosphate to overcome poor enzyme binding. Dr. Antonio Costantini documented remarkable improvements in fibromyalgia, Parkinson's, and chronic fatigue using 600-1800mg daily, with some patients requiring exactly 1800mg while lower doses provided no benefit.
The research reveals that many common medications including metformin, antibiotics, and antidepressants block thiamine transporters, creating iatrogenic functional deficiency even with adequate dietary intake. This helps explain why some people develop mysterious fatigue and neurological symptoms while on certain medications, and why megadose thiamine can reverse these effects when standard supplementation fails.
The deeper question: Why are the enzymes damaged?
Here's where the conversation needs to shift. While megadosing genuinely helps people – and many practitioners recommending it are doing their best with the tools they understand – it's essentially using nutrients as medication to bypass dysfunction rather than asking why that dysfunction exists.
The research points to clear causes of enzyme damage that rarely get addressed:
Oxidative stress damages enzyme structure and function, but this oxidative stress often stems from poor antioxidant status. Why poor antioxidant status? Because fat-soluble vitamins A, E, and CoQ10 aren't being absorbed. Why aren't they absorbed? Poor bile flow prevents fat digestion and fat-soluble vitamin absorption. Yet how many people taking 1800mg of thiamine have addressed their bile flow first?
Chronic inflammation from gut dysfunction directly impairs mitochondrial enzymes. This inflammation exists because pathogenic bacteria thrive in an alkaline small intestine. The small intestine becomes alkaline when? When stomach acid is insufficient and bile flow is poor – bile is one of our primary antimicrobial defenses in the small intestine. Without proper pH and bile, the gut becomes a source of endotoxins that damage mitochondria throughout the body.
Heavy metal accumulation, particularly copper excess, directly inhibits thiamine-dependent enzymes. Copper accumulates when bile flow is poor (bile is a major excretion route), when zinc is deficient (zinc opposes copper), and when molybdenum is insufficient (molybdenum binds copper for excretion). The same digestive dysfunction preventing nutrient absorption also prevents toxin excretion.
The uncomfortable truth? Those damaged enzymes requiring megadose nutrients are often damaged because foundational systems – digestion, detoxification, and circulation – are profoundly compromised. The megadose works by overriding the damage through sheer concentration, but it doesn't repair the enzymes or address why they're damaged.
The metabolic domino effect: How separate systems create unified dysfunction
Research exposes profound interconnections between seemingly unrelated metabolic pathways. Poor bile flow impairs fat digestion, reducing absorption of fat-soluble vitamins A, D, E, and K – all essential for mitochondrial function. Without vitamin E protecting mitochondrial membranes from oxidation, without vitamin D regulating calcium handling, and without vitamin K supporting electron transport, energy production falters regardless of other interventions.
The histamine-copper-methylation triangle creates particularly vicious cycles. High copper damages the DAO enzyme that breaks down histamine, leading to histamine intolerance and chronic inflammation. Elevated histamine depletes methyl groups needed for detoxification, while inflammation further impairs methylation. Meanwhile, poor methylation reduces phosphatidylcholine production needed for bile, completing the circle back to impaired fat digestion and vitamin deficiencies.
Vitamin B6 deficiency triggers multiple simultaneous failures: increased oxalate production (which binds minerals and damages mitochondria), reduced glutathione synthesis (compromising detoxification), and impaired histamine breakdown. Each pathway failure worsens the others, creating self-perpetuating dysfunction that explains why addressing single pathways rarely succeeds.
The molybdenum-copper interaction represents a critical but overlooked factor. Molybdenum binds excess copper and facilitates its excretion while supporting sulfite oxidase for detoxification. Without adequate molybdenum, copper accumulates, creating oxidative stress, estrogen dominance, and enzyme dysfunction throughout multiple systems. This single mineral imbalance can trigger cascading failures across histamine, methylation, and energy pathways.
Light, timing, and digestion shape mitochondrial destiny
Circadian rhythms directly control mitochondrial biogenesis and function through clock proteins that regulate when mitochondrial genes are expressed. Research shows that most mitochondrial proteins peak during early daylight hours, with substrate-specific rhythms optimizing different fuel sources throughout the day. Disrupting these rhythms through irregular light exposure or meal timing directly impairs energy production efficiency.
Natural sunrise and sunset light exposure provides the primary signal synchronizing these rhythms. Light suppresses melatonin, which accumulates in mitochondria at concentrations 1000 times higher than blood levels, where it directly protects against oxidative damage and regulates mitochondrial dynamics. Even dim light at night (3-200 lux) can shift these rhythms and create metabolic dysfunction.
Stomach acid represents an underappreciated lynchpin of mitochondrial health. Hypochlorhydria (low stomach acid) creates cascading problems: poor protein digestion limits amino acids for mitochondrial protein synthesis, reduced mineral absorption depletes iron and zinc needed for respiratory complexes, and impaired B12 absorption disrupts fatty acid oxidation. The resulting small intestinal bacterial overgrowth produces endotoxins that directly damage mitochondria while consuming nutrients meant for the host.
Research demonstrates that red and near-infrared light therapy (630-850nm wavelengths) directly enhances mitochondrial function by activating cytochrome c oxidase, increasing ATP production by 15-25% in treated cells. This photobiomodulation also stimulates mitochondrial biogenesis and reduces oxidative stress, providing a direct method to support cellular energy independent of nutritional pathways.
The partial knowledge trap: Why incomplete approaches guarantee failure
People commonly get stuck in treatment loops because they address visible symptoms without understanding underlying connections. Taking antihistamines without supporting bile production fails because poor bile flow creates the alkaline intestinal environment where histamine-producing bacteria thrive. Supporting methylation without addressing mineral imbalances fails because copper excess blocks the very enzymes methylation support tries to enhance.
The supplement industry inadvertently perpetuates these failures through fragmentation – no manufacturer has more than 7% market share, creating a landscape of competing single-solution products rather than comprehensive system support. Medical specialization compounds the problem, with gastroenterologists treating the gut, endocrinologists managing hormones, and psychiatrists addressing mood, while missing that these symptoms often stem from the same mitochondrial dysfunction.
Many practitioners sharing partial solutions aren't trying to mislead – they've found something that helped (maybe megadose thiamine, maybe methylation support) and genuinely want others to experience relief. But partial understanding creates partial solutions. The thiamine expert might not understand bile, the methylation specialist might not grasp mineral ratios, and each shares their piece without seeing the whole picture.
Research reveals that biological systems don't have single rate-limiting steps but rather multiple control points that shift based on conditions. This explains why taking CoQ10 alone rarely fixes fatigue – if iron is low, B-vitamins are depleted, or membranes are damaged, adding one cofactor simply moves the bottleneck elsewhere. Success requires coordinated support across multiple pathways simultaneously.
Why bypassing becomes the strategy instead of restoration
The megadose approach has become standard because it genuinely works – in the sense that it forces function through damaged systems. For someone suffering from severe chronic fatigue, taking 1800mg of thiamine that provides relief is absolutely valid. Sometimes we need to stop the bleeding before we can heal the wound.
But somewhere along the way, the bypass became the permanent strategy rather than a temporary bridge. Why? Several factors converge:
Complexity doesn't sell. "Fix your fatigue with high-dose thiamine" gets more attention than "spend six months systematically rebuilding your digestive function." Quick fixes spread faster than foundational work, even among well-intentioned practitioners.
Research funding favors single interventions. Studies show megadoses work, so they get recommended. But studies rarely ask, "What if we fixed the bile flow first?" because that's not how research grants work. We study isolated variables, not systems restoration.
Foundational work is unglamorous. Supporting stomach acid with betaine HCl, optimizing bile flow with ox bile or bitter herbs, balancing minerals over months – none of this is as exciting as the latest mitochondrial enhancement supplement. Yet these boring basics determine whether those sophisticated supplements can even work.
Patients are often too depleted for foundational work initially. Someone in severe dysfunction might need the megadose support just to function well enough to address foundations. This is reasonable, but the temporary intervention often becomes permanent dependence.
Breaking free from the vicious cycles
The research points toward a clear but counterintuitive conclusion: successful mitochondrial restoration requires doing many things partially right rather than one thing perfectly. This means simultaneously supporting bile flow for fat-soluble vitamin absorption, optimizing stomach acid for mineral absorption, balancing copper and zinc ratios, providing comprehensive B-vitamin cofactors, managing histamine through DAO support, ensuring adequate molybdenum for copper detoxification, and aligning circadian rhythms through proper light exposure.
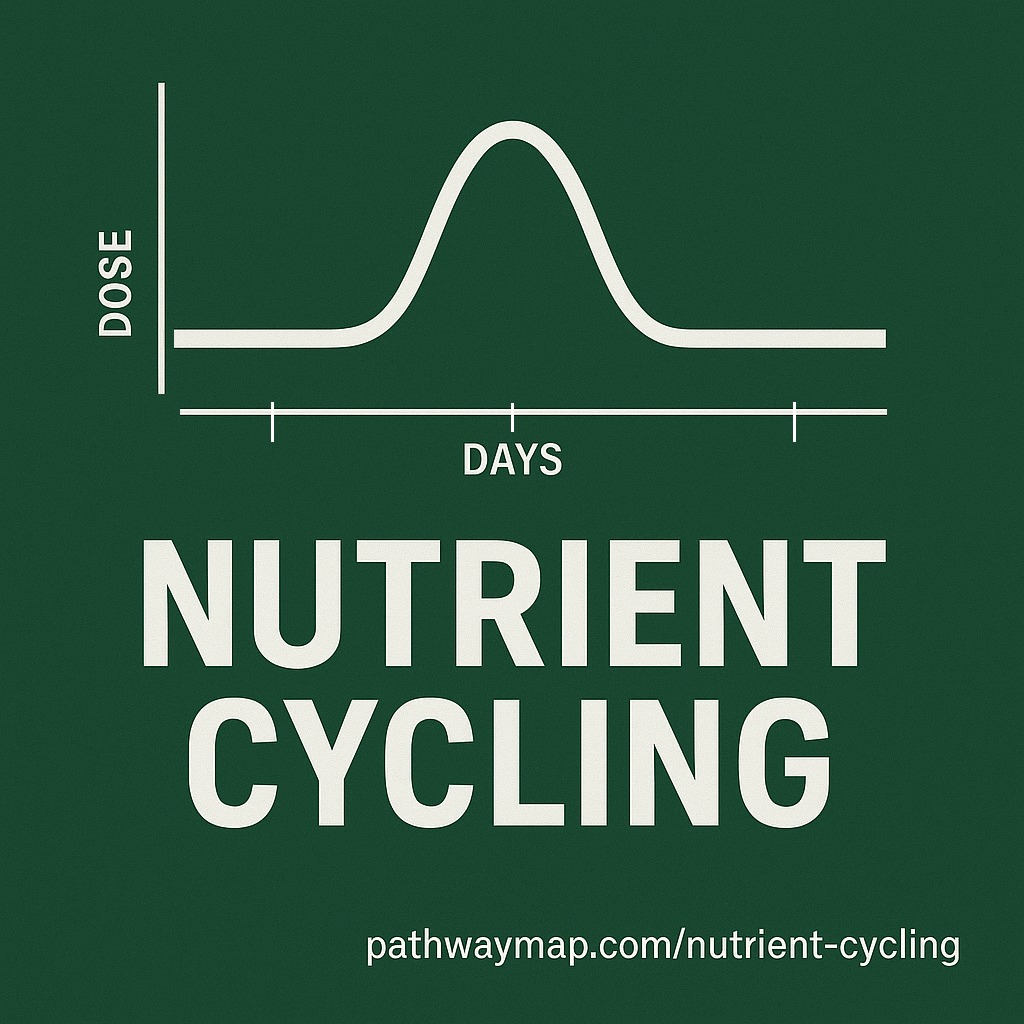
The concept of functional deficiency explains why megadosing often succeeds where normal supplementation fails – damaged or inhibited enzymes require cofactor concentrations far above normal to restore function. This isn't about correcting nutritional deficiency but rather using nutrients as pharmacological agents to bypass metabolic blocks. Yet this bypass doesn't repair the enzymes or address the damage source.
Understanding these interconnections reveals why fragmented health information keeps people stuck. When each specialist or supplement company promotes their piece without acknowledging the larger web, patients bounce between partial solutions that may even worsen other aspects of the dysfunction. The histamine expert doesn't mention bile, the methylation specialist ignores minerals, and the mitochondrial supplement doesn't address digestion.
The path forward: Restoration over override
What would it look like to actually restore normal enzyme function instead of overriding it? The research and clinical experience point to a systematic approach:
First, establish rhythm. Get morning sunlight in your eyes. Watch the sunset. Create consistent meal times. This costs nothing but attention, yet it synchronizes thousands of cellular processes that no supplement can correct.
Second, restore digestion. Support stomach acid (betaine HCl, apple cider vinegar, zinc). Optimize bile flow (taurine, glycine, bitter herbs, phosphatidylcholine). This isn't glamorous, but it determines whether any other intervention can succeed.
Third, balance minerals. Test, don't guess. Address copper excess with zinc and molybdenum. Ensure adequate magnesium. Support trace minerals. This takes patience – minerals move slowly but affect every enzyme in your body.
Fourth, remove obstacles. Identify and eliminate food sensitivities. Address chronic infections. Reduce toxic exposures. Support detoxification pathways once bile flow is restored. This is detective work, not quick fixes.
Finally, nourish comprehensively. Once digestion works and minerals balance, normal doses of nutrients often suffice. The enzymes begin functioning normally again because the damage sources are removed and repair is supported.
Conclusion
Mitochondrial health emerges not from any single intervention but from recognizing and supporting the complex metabolic web that conventional medicine's reductionist approach systematically fragments. The body operates as an integrated system where circadian rhythms, digestive function, mineral balance, and metabolic pathways all influence cellular energy production. Success requires moving beyond the "find and fix the deficiency" model to understand functional impairments, metabolic blocks, and system-wide interactions.
The prevalence of high-dose thiamine use represents patients intuitively discovering what research now confirms – that metabolic dysfunction often requires cofactor saturation to overcome enzymatic impairments rather than simple deficiency correction. But this discovery should prompt us to ask why the impairments exist, not simply accept them as permanent.
For those seeking to restore mitochondrial function, the path forward requires embracing complexity while maintaining systematic approach: establish circadian rhythm through proper light exposure, optimize digestion starting with stomach acid and bile, balance minerals with attention to copper-zinc-molybdenum interactions, support all pathways simultaneously with comprehensive cofactors, and recognize that healing happens not through finding the single solution but through patiently nurturing the entire system back to balance.
The mitochondria evolved not as isolated energy factories but as integrated components of a unified biological network. Healing them requires honoring that integration – not through more sophisticated overrides, but through humble attention to the foundations everyone steps over in their rush toward the next breakthrough.
Sources
- The Mitochondrion – Molecular Biology of the Cell – NCBI Bookshelf
- Biochemistry, Citric Acid Cycle – StatPearls – NCBI Bookshelf
- Role of Cardiolipin in Mitochondrial Function and Dynamics – PMC
- Beyond Deficiency: Using Thiamine as a Metabolic Stimulant – Hormones Matter
- High-dose thiamine improves the symptoms of fibromyalgia – PMC
- Thiamine – MEpedia
- Physiology, Bile Secretion – StatPearls – NCBI Bookshelf
- Molybdenum for Copper Toxicity — Mineral Balancing
- Manage Histamine Intolerance with Methylation & Nutrient Therapy
- Marginally Insufficient Thiamine Intake and Oxalates – Hormones Matter
- Circadian control of oscillations in mitochondrial rate-limiting enzymes – PNAS
- Systematic review of light exposure impact on human circadian rhythm
- Hypochlorhydria (Low Stomach Acid) – Cleveland Clinic
- Red Light Therapy and Mitochondria for ATP Production
- Cashing in on the booming market for dietary supplements – McKinsey
- Rate-limiting step (biochemistry) – Wikipedia
- Mega-Dose Thiamine: Beyond Addressing "Deficiency" – EONUTRITION
- Vitamins and Minerals for Energy, Fatigue and Cognition – PMC
- Mitochondrial function and toxicity: Role of B vitamins – ScienceDirect
- Coenzyme Q10 in the Treatment of Mitochondrial Disease – Sage Journals