The formation of iodolipids represents a sophisticated enzymatic process with significant implications for human health, requiring iodine doses far exceeding typical dietary intakes. These specialized molecules, particularly 6-iodolactone and 2-iodohexadecanal, emerge through specific biochemical pathways and demonstrate potent biological activities ranging from thyroid autoregulation to selective cancer cell toxicity.
Enzymatic Machinery Driving Iodolipid Synthesis
The biochemical pathways governing iodolipid formation center on a family of peroxidase enzymes that orchestrate the incorporation of iodine into polyunsaturated fatty acids. Thyroid peroxidase (TPO), lactoperoxidase (LPO), and myeloperoxidase (MPO) serve as the primary catalysts, utilizing hydrogen peroxide to generate reactive iodine species that attack carbon-carbon double bonds in fatty acid substrates.
The formation of 6-iodolactone (6-IL) from arachidonic acid follows a precise enzymatic mechanism. In the presence of iodide and hydrogen peroxide, peroxidases generate an enzyme-bound iodinating species – not free molecular iodine, but likely hypoiodous acid or enzyme-bound hypoiodite. This reactive intermediate attacks the double bonds of arachidonic acid, leading to the formation of 6-iodo-5-hydroxy-8,11,14-eicosatrienoic acid, which cyclizes to form the characteristic δ-lactone structure. The reaction exhibits strict pH optima around 6-7 and is specifically inhibited by methimazole, confirming its enzymatic nature.
The synthesis of 2-iodohexadecanal (2-IHDA) follows a different pathway, targeting the vinyl ether groups of plasmalogens – specialized ether-linked phospholipids abundant in cell membranes. Lactoperoxidase-catalyzed iodination attacks these vinyl ether bonds in plasmenylethanolamine, producing 2-IHDA, which thyroid cells can further reduce to 2-iodohexadecan-1-ol through aldehyde-reducing enzymes. This conversion ratio depends on hydrogen peroxide levels and iodide concentration, reflecting the complex regulatory mechanisms governing iodolipid metabolism.
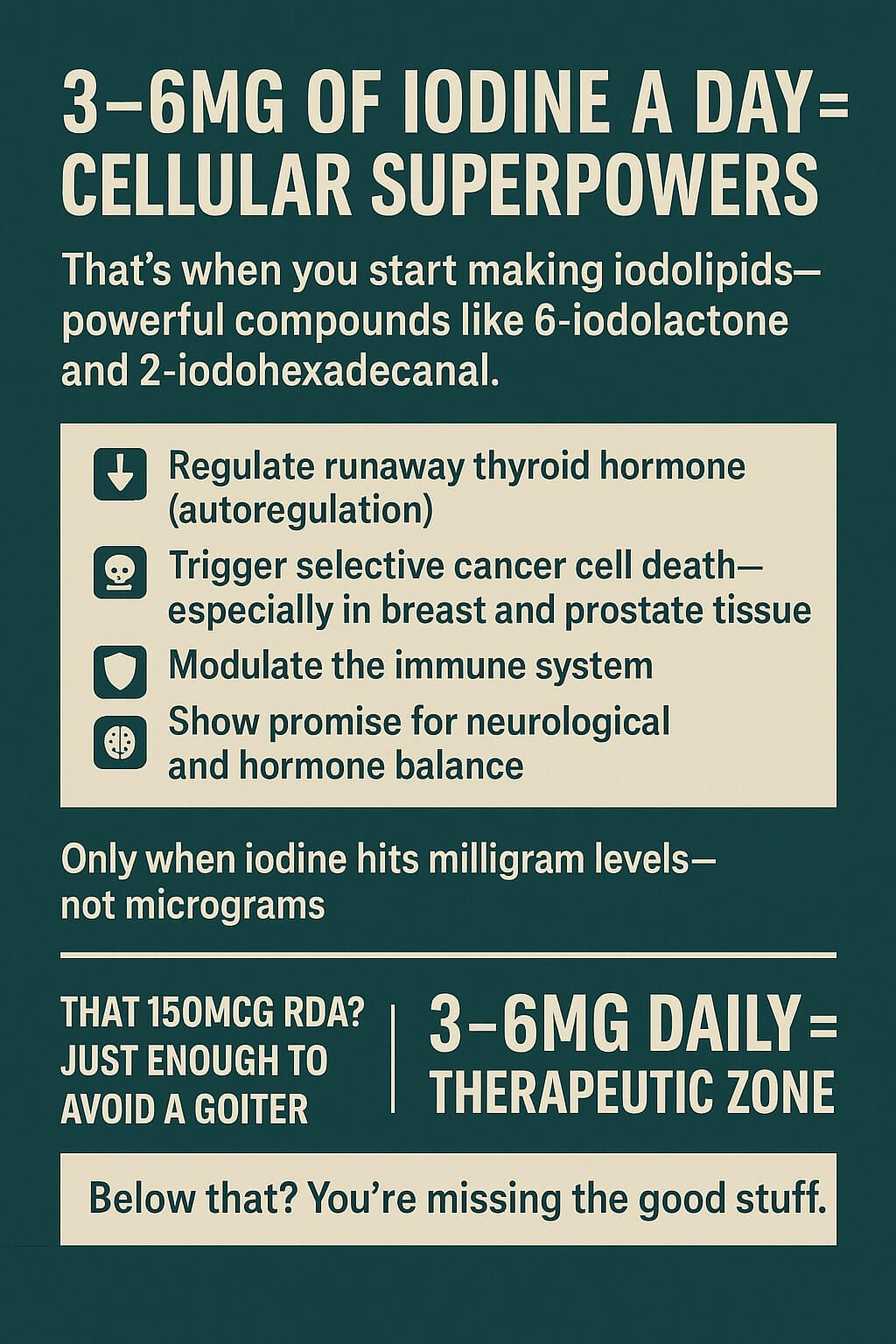
Dose Thresholds Reveal Non-Linear Biology
The relationship between iodine intake and iodolipid formation defies simple linear models, instead demonstrating clear threshold effects around 3 milligrams per day. Below this level, minimal iodolipid synthesis occurs despite adequate iodine for basic thyroid hormone production. This threshold finding emerged from multiple lines of evidence, including clinical trials showing no effect at 1.5mg daily but significant biological responses at 3-6mg daily doses.
The frequently cited 12.5mg dose represents a therapeutic threshold established through clinical practice rather than a minimum requirement. This dose, containing 5mg molecular iodine and 7.5mg iodide, derives from historical French medical protocols and modern clinical experience. Japanese populations consuming 1-3mg daily from seaweed demonstrate enhanced tissue iodine levels and lower rates of certain cancers, supporting the relevance of milligram-range intakes for extrathyroidal benefits.
Cell culture studies provide mechanistic insight into these thresholds. Breast cancer cells require 20-200 μM molecular iodine concentrations to induce significant changes in gene expression and growth inhibition, while the bioactive 6-iodolactone shows effects at lower concentrations of 5-10 μM. This difference reflects the amplification achieved through enzymatic conversion of iodine to more potent iodolipid mediators.
Widespread Tissue Production Challenges Thyroid-Centric Views
While the thyroid gland represents the primary site of iodolipid synthesis, research reveals extensive extrathyroidal production capacity across multiple organs. Mammary tissue demonstrates particularly robust iodolipid synthesis, especially during lactation and pregnancy when sodium-iodide symporter expression increases dramatically. This enhanced capacity likely serves protective functions for both maternal and infant health.
Prostate tissue, both normal and malignant, actively produces iodolipids with 50-70% of adenocarcinomas expressing functional iodine uptake mechanisms. Salivary glands, gastric mucosa, and other epithelial tissues also demonstrate iodolipid synthesis capacity, suggesting evolutionary conservation of these pathways beyond thyroid function. The widespread distribution implies that many tissues may suffer functional deficits when dietary iodine remains at levels sufficient only for thyroid hormone production.
The cellular machinery for iodolipid synthesis localizes primarily to cell membranes where peroxidase activity concentrates. Synthesis requires coordinated expression of iodine transporters, peroxidase enzymes, and hydrogen peroxide generating systems like DUOX1 and DUOX2. This complex enzymatic infrastructure explains why simple iodine supplementation at low doses fails to achieve therapeutic effects – the entire biosynthetic apparatus must be adequately supplied with substrate to function optimally.
Safety Profile Supports Therapeutic Applications
Clinical trials and population studies provide reassuring safety data for iodine supplementation in the milligram range. The therapeutic window of 1-6mg daily molecular iodine demonstrates minimal adverse effects in healthy individuals while providing documented benefits for conditions like fibrocystic breast disease and benign prostatic hyperplasia. Studies lasting up to two years at these doses showed no significant thyroid dysfunction or other serious adverse events.
The FDA’s upper tolerable limit of 1.1mg daily appears conservative given international experience. Japanese populations routinely consume 1-3mg daily without increased thyroid disease incidence, and clinical trials using 3-6mg daily report primarily minor, reversible side effects like transient acne or mild gastrointestinal symptoms. However, certain populations require careful monitoring, including those with pre-existing thyroid nodules, autoimmune thyroid disease, or concurrent use of lithium or amiodarone.
At doses exceeding 6mg daily, the risk-benefit ratio shifts. Some individuals experience transient hypothyroidism, headaches, or metallic taste at 9-12mg daily doses. The classical Wolff-Chaikoff effect, mediated by iodolipids themselves, provides an autoregulatory mechanism preventing acute thyroid toxicity, but chronic high-dose exposure may overwhelm these protective systems.
Expanded Iodolipid Repertoire Reveals Therapeutic Diversity
Beyond the well-characterized 6-iodolactone and 2-iodohexadecanal, research identifies an expanding family of bioactive iodolipids. Docosahexaenoic acid undergoes iodination to form 5-iodo-4-hydroxy-docosapentaenoic acid γ-lactone, while multiple positional isomers of iodinated arachidonic acid demonstrate varying biological activities. Each double bond in polyunsaturated fatty acids represents a potential iodination site, creating combinatorial diversity in iodolipid structures.
Synthetic iodolipid analogs like 12-iododecanoic acid and 16-iodo-9-hexadecenoic acid serve as molecular probes for studying fatty acid metabolism and protein modifications. These compounds maintain biological activity similar to their non-iodinated counterparts while enabling tracking through radioiodine labeling or mass spectrometry detection.
The structural diversity of iodolipids translates to functional diversity. While 6-iodolactone acts primarily as a potent PPARγ agonist with six-fold higher affinity than arachidonic acid, 2-iodohexadecanal functions in thyroid autoregulation by inhibiting NADPH oxidase and thyroid peroxidase. This functional specialization suggests that different tissues may produce distinct iodolipid profiles tailored to their physiological requirements.
Selective Cancer Toxicity Offers Therapeutic Promise
The most compelling therapeutic application of iodolipids lies in their selective toxicity toward cancer cells. Malignant cells typically contain 4-5 times higher arachidonic acid concentrations than normal cells, providing enhanced substrate for 6-iodolactone formation when adequate iodine is supplied. This biochemical difference enables preferential iodolipid accumulation in tumors, fulfilling criteria for targeted therapy.
Clinical and preclinical evidence supports anti-cancer efficacy across multiple tumor types. Mammary cancer models show 62.5% tumor incidence with iodine supplementation versus 100% in controls, accompanied by significant size reductions in established tumors. Breast cancer cells undergo apoptosis at 10-20 μM molecular iodine concentrations, while normal breast epithelial cells require 40 μM for similar effects – a two-fold therapeutic window.
The mechanisms underlying anti-cancer effects extend beyond simple cytotoxicity. Iodolipids induce differentiation programs in cancer cells, increasing expression of differentiation markers while decreasing stem cell-like populations. They enhance chemotherapy effectiveness by preventing drug efflux and reducing chemoresistant subpopulations. Anti-angiogenic effects, mediated through VEGF suppression, further contribute to tumor growth inhibition.
Clinical Translation Requires Precision Dosing
The transition from laboratory findings to clinical practice demands careful attention to dosing strategies. For cancer prevention and treatment adjuvant therapy, doses of 3-6mg daily molecular iodine appear optimal based on current evidence. This range achieves therapeutic tissue concentrations while minimizing adverse effects. Fibrocystic breast disease responds well to similar doses, with over 65% of patients experiencing clinically significant improvement.
The form of iodine matters critically for extrathyroidal effects. Molecular iodine (I₂) demonstrates superior efficacy compared to iodide (I⁻) for iodolipid formation in breast and other extrathyroidal tissues. This distinction likely reflects differential uptake mechanisms, with molecular iodine utilizing facilitated diffusion pathways evolutionarily conserved from marine algae, while iodide depends on sodium-iodide symporter expression.
Timing and duration considerations also influence outcomes. Loading doses of 12.5-50mg daily for several weeks may accelerate tissue saturation, followed by maintenance doses of 3-12.5mg daily. The prolonged half-life of iodine in extrathyroidal tissues supports intermittent dosing strategies, though optimal protocols await further clinical validation.
Future Directions in Iodolipid Research
The field of iodolipid biology stands at an inflection point between basic discovery and clinical translation. Critical questions remain regarding optimal dosing for specific conditions, biomarkers for monitoring therapeutic response, and potential drug interactions. The development of iodolipid analogs with enhanced stability or tissue selectivity could improve therapeutic indices.
Understanding individual variation in iodolipid synthesis capacity may enable personalized dosing strategies. Genetic polymorphisms in peroxidase enzymes, iodine transporters, or fatty acid metabolism pathways likely influence therapeutic responses. Integration with systems biology approaches could reveal how iodolipids interact with other signaling networks to modulate cellular fate decisions.
The broader implications of widespread iodolipid deficiency in Western populations deserve consideration. If milligram-range iodine intakes are required for optimal extrathyroidal function, current dietary recommendations may need revision. The Japanese experience suggests that sustained higher intakes are both safe and potentially beneficial, challenging conventional wisdom about iodine sufficiency defined solely by thyroid parameters.
Iodolipid formation represents a fundamental biochemical process with ramifications extending far beyond thyroid physiology. The requirement for milligram rather than microgram doses of iodine reflects the substantial substrate demands of extrathyroidal iodolipid synthesis. As our understanding of these remarkable molecules expands, so too does the potential for therapeutic applications addressing some of our most challenging health conditions. The key lies in recognizing that evolution equipped our cells with sophisticated iodine-handling machinery for purposes beyond thyroid hormone – purposes we are only beginning to appreciate and harness for human health.