TSH commonly increases temporarily when people boost their iodine intake due to complex autoregulatory mechanisms that protect the thyroid from producing excess hormones. This elevation, typically lasting weeks to months, occurs as the thyroid adapts to new iodine levels through the Wolff-Chaikoff effect and other protective processes. While usually benign and self-limiting in healthy individuals, certain populations face higher risks of persistent dysfunction.
The Wolff-Chaikoff Effect Drives Initial TSH Elevation
The Wolff-Chaikoff effect represents the thyroid’s immediate defensive response to high iodine levels. When intracellular iodide concentrations exceed 10⁻³ molar, thyroid peroxidase (TPO) activity becomes directly inhibited through formation of inhibitory compounds including iodolactones and iodoaldehydes. This acute autoregulatory mechanism blocks the organification of iodide within thyroid follicles, effectively halting thyroid hormone production within hours to days of increased iodine exposure.
The molecular cascade involves several interconnected processes. High iodide concentrations interfere with hydrogen peroxide generation required for TPO activity, while simultaneously disrupting calcium signaling pathways that normally support TSH action. The reaction I⁻ + I₂ ⇌ I₃⁻ at elevated iodide levels sequesters molecular iodine, further disrupting normal organification processes. As thyroid hormone synthesis decreases, even slight reductions in circulating T4 and T3 trigger compensatory TSH increases through normal hypothalamic-pituitary feedback mechanisms.
Most individuals “escape” from the Wolff-Chaikoff effect within 10-14 days through downregulation of the sodium iodide symporter (NIS). This adaptation reduces intracellular iodide below the critical inhibitory threshold, allowing organification to resume. The escape mechanism involves post-transcriptional NIS regulation through the PI3K/Akt pathway and reactive oxygen species production. However, certain populations—including those with Hashimoto’s thyroiditis, elderly individuals, and fetuses—may fail to escape, leading to persistent TSH elevation.
Beyond the Wolff-Chaikoff effect, additional autoregulatory mechanisms contribute to TSH changes. Prolonged high iodine intake significantly inhibits type 2 deiodinase (D2) activity in the pituitary and hypothalamus by 25-70%, without affecting D2 mRNA or protein expression. This post-translational modification reduces local T3 production where it matters most for TSH regulation. The resulting impaired hypothalamic T3 production leads to increased TRH synthesis, while reduced pituitary T3 causes TSH hypersecretion despite potentially normal circulating thyroid hormone levels.
Timeline Reveals Distinct Phases of Adaptation
The physiological response to increased iodine follows a predictable timeline across three distinct phases. During the acute phase (hours to days), TPO inhibition begins within hours of high iodine exposure, with the Wolff-Chaikoff effect reaching maximum organification blockade by days 2-3. Initial TSH rises occur within 24-48 hours as the pituitary responds to declining hormone synthesis.
The adaptation phase (days to weeks) sees NIS downregulation beginning within 2-3 days and peaking at 7-10 days. Most healthy individuals successfully escape the Wolff-Chaikoff effect by days 10-14, with TSH beginning to normalize after 2-3 weeks in those who adapt successfully. Deiodinase inhibition becomes significant after 1-2 weeks of sustained excess intake, potentially prolonging TSH elevation even after escape from the initial effect.
During the chronic phase (weeks to months), TSH may remain elevated for extended periods during iodine repletion in previously deficient individuals. Multiple organs including the thyroid, breast, prostate, and salivary glands compete for iodide until achieving saturation. Complete thyroidal and extrathyroidal iodine repletion typically requires 3-6 months. The Danish DanThyr study documented population-level TSH increases from 1.27 to 1.38 mU/L over an 11-year follow-up period after salt iodization, demonstrating the gradual nature of adaptation.
Clinical studies have captured these timelines in detail. Paul et al. showed significant TSH increases within 14 days at 1,500 μg daily doses, while the Clark kelp supplementation study documented persistent TSH elevation throughout a 4-week treatment period, with most values returning to baseline within 2 weeks after cessation. The timeline varies substantially based on baseline iodine status, with severely deficient individuals showing more prolonged adaptation periods.
Normal Adaptation Differs Markedly from Pathological Responses
Normal TSH adaptation during iodine repletion exhibits specific characteristics that distinguish it from concerning reactions. Expected TSH increases are typically modest, with population medians rising from approximately 1.2-1.3 mU/L to 1.4-1.5 mU/L after iodine fortification programs. Individual TSH elevations during normal adaptation generally remain below 4.5 mU/L, with free T4 and free T3 levels staying within normal reference ranges. Crucially, normal adaptation is asymptomatic—individuals experience no hypothyroid symptoms like fatigue, weight gain, or cold intolerance.
Pathological responses present distinctly different patterns. TSH levels exceeding 10 mU/L consistently indicate pathological hypothyroidism requiring treatment, particularly when accompanied by declining free T4 levels. TSH elevation persisting beyond 6 months after initiating appropriate iodine supplementation suggests underlying thyroid dysfunction rather than normal adaptation. The development of clinical symptoms, new or increasing thyroid antibodies, or thyroid enlargement all indicate pathological rather than physiological responses.
The distinction between transient subclinical hypothyroidism and true hypothyroidism proves critical for clinical management. Transient subclinical hypothyroidism during adaptation typically features TSH levels between 4.5-10 mU/L with normal free hormones, remains asymptomatic, stabilizes over 3-6 months, and shows negative or stable thyroid antibodies. True hypothyroidism, conversely, demonstrates progressive TSH elevation often exceeding 10 mU/L, declining free T4 levels, clinical symptoms, and frequently positive or rising TPO antibodies.
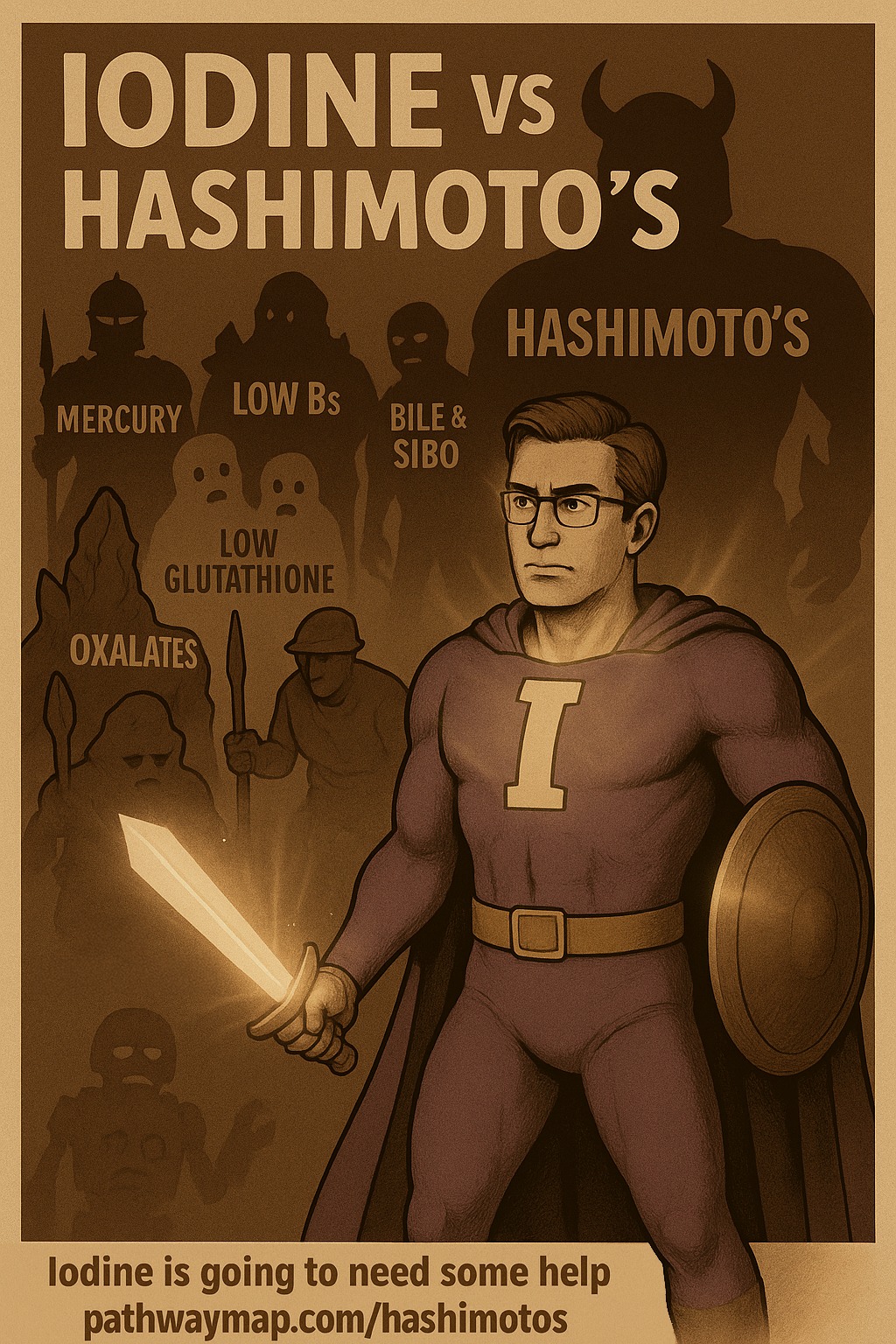
Special Populations Face Elevated Risks
Hashimoto’s thyroiditis patients show extreme sensitivity, with studies documenting thyroid dysfunction at doses as low as 250 μg daily. One case report described TSH rising to 98 mIU/L with antibodies increasing to 9,800 after just 3 months of supplementation. The mechanism involves iodine stimulating thyroid peroxidase production, triggering increased TPO antibodies and autoimmune flare-ups.
Individuals with nodular goiter or autonomous thyroid nodules face risk of the Jod-Basedow phenomenon, where pre-existing nodules with ineffective iodine autoregulation can precipitate life-threatening hyperthyroidism. A documented case involved a 50-year-old woman with multinodular goiter who developed thyroid storm after taking 30,000 μg daily, requiring intensive care and renal replacement therapy.
Elderly populations demonstrate increased susceptibility due to age-related changes in thyroid physiology. TSH levels naturally increase with age, and elderly individuals show less circadian variation in TSH with weaker TRH responses. Even mild iodine-induced hyperthyroidism in those over 65 requires treatment due to cardiovascular complications including atrial fibrillation and heart failure.
Pregnant women present unique concerns as the fetal thyroid cannot escape the Wolff-Chaikoff effect until approximately 36 weeks gestation. Studies show a 2.5-fold increased risk of TSH exceeding 3 mIU/L in women consuming 200 μg or more daily versus less than 100 μg. Excessive maternal iodine can cause fetal goiter, neonatal airway obstruction, and congenital hypothyroidism.
Warning signs that TSH elevation represents a problem rather than normal adaptation include values persistently exceeding 10 mIU/L, rising TPO antibodies above 35 IU/mL, development of hypothyroid symptoms, and urinary iodine levels exceeding 300 μg/L. The American Thyroid Association recommends avoiding iodine supplements exceeding 500 μg daily in the general population, with a tolerable upper limit of 1,100 μg daily for adults.
Clinical Evidence Documents Predictable Dose-Response Patterns
Extensive clinical research has established clear dose-response relationships between iodine intake and TSH changes. Paul et al.’s controlled trial with 30 healthy volunteers demonstrated that 1,500 μg daily caused significant TSH increases with compensatory T4/T3 decreases, while 500 μg and 250 μg daily produced no significant changes, with all values remaining within normal ranges despite the elevations.
The Clark kelp supplementation study revealed dose-dependent effects in a double-blind, placebo-controlled trial of 36 healthy subjects. Low-dose kelp produced significant TSH increases (P = 0.04), while high-dose kelp caused more pronounced elevation (P = 0.002) with enhanced TRH stimulation responses. Notably, TSH values returned to baseline within 2 weeks after cessation, except in the high-dose group where TSH remained significantly decreased.
Population-level studies provide crucial long-term data. The Danish DanThyr study followed 2,203 individuals for 11 years after salt iodization began in 2000. Areas with highest iodine intake showed TSH increases from 1.30 to 1.49 mU/L (P < 0.001), while low iodine areas showed no significant increase. Tasmania’s analysis of 1.66 million TSH assessments from 1995-2013 documented a 62.3% decline in severe TSH suppression and 59.7% decline in severe elevation following iodine fortification, though borderline TSH elevation above 4.0 mIU/L showed an increasing trend.
Monitoring Requires Systematic Laboratory Assessment
Clinical monitoring during iodine repletion follows established protocols based on risk stratification. The American Thyroid Association recommends baseline assessment including TSH, free T4, and TPO antibodies before initiating supplementation. Primary monitoring tests include TSH as the most sensitive screening test, free T4 to distinguish clinical from subclinical dysfunction, and free T3 only when TSH is abnormal but free T4 appears inappropriately normal.
Monitoring frequency varies by population and clinical scenario. For the general adult population with normal baseline results, no routine re-testing is needed unless clinical changes occur. High-risk populations require more intensive monitoring: pregnant women need TSH assessment every 4-6 weeks during the first half of pregnancy and at least once at 26-32 weeks. Individuals with Hashimoto’s thyroiditis or other autoimmune conditions should undergo testing at 6-8 weeks initially, then every 3 months until stable.
The World Health Organization employs population-level indicators including urinary iodine concentration, with targets of 100-199 μg/L for school-age children and 150-249 μg/L for pregnant women. Thyroglobulin serves as a long-term marker, with elevated levels indicating deficiency. These multi-indicator approaches combine urinary iodine, thyroglobulin, TSH levels, and thyroid volume assessments to evaluate iodine nutrition status comprehensively.
Iodine Sufficiency Correction Produces Different Effects Than Excess
The physiological impact of correcting iodine deficiency differs fundamentally from the effects of iodine excess. During iodine sufficiency correction from mild-moderate deficiency to adequate levels, a U-shaped relationship emerges where TSH increases from deficiency levels as iodine status improves toward sufficiency. Previously enlarged, hyperplastic thyroid glands reduce in size, requiring higher TSH stimulation for equivalent hormone production. Each remaining thyrocyte requires stronger TSH stimulation for optimal function as the gland’s autoregulatory mechanisms reset to new iodine availability levels.
Excess iodine effects involve distinctly pathological mechanisms. TSH elevation results from the Wolff-Chaikoff effect, NIS downregulation, and deiodinase inhibition at doses exceeding 750 μg daily in children and 1,700 μg daily in adults. Individuals with underlying thyroid autoimmunity, including Hashimoto’s thyroiditis or previous Graves’ disease, show increased likelihood of developing persistent hypothyroidism. The dose-dependent response correlates directly with the degree of iodine excess.
Population studies illustrate these differences clearly. Areas transitioning from deficiency to sufficiency show gradual TSH normalization over years, while populations exposed to excess iodine demonstrate more acute changes. The Moroccan iodine supplementation study showed TSH decreases and improved lipid profiles after 6 months of repletion in a deficient population, contrasting with studies of excess exposure showing TSH increases and potential dysfunction.
Selenium and Other Cofactors Play Critical Roles
Selenium emerges as the most critical cofactor for thyroid function during iodine repletion. This trace element forms an essential component of deiodinase enzymes (DIO1, DIO2, DIO3) responsible for converting T4 to active T3. Selenium-containing glutathione peroxidases protect the thyroid from hydrogen peroxide damage during hormone synthesis, while thioredoxin reductases provide additional antioxidant protection.
Clinical evidence supports selenium’s importance. Supplementation with 200 μg daily selenomethionine decreased TPO antibodies and improved thyroid ultrasound structure in Hashimoto’s thyroiditis patients. European guidelines include 6-month selenium treatment for mild Graves’ orbitopathy. During pregnancy, 200 μg selenium reduced autoimmune thyroid dysfunction risk.
A critical finding concerns supplementation sequencing: iodine adequacy must be established before selenium supplementation to prevent severe hypothyroidism. Severe combined deficiency can cause myxedematous cretinism, while selenium deficiency may paradoxically protect against iodine-induced thyrotoxicosis in severely iodine-deficient populations.
Other essential cofactors include iron, required for heme-dependent thyroid peroxidase activity. Iron supplementation at 60 mg four times weekly improved iodized salt efficacy in iron-deficient children with goiter. Iron deficiency and goiter coexist in up to 25% of children in some regions. Vitamin A influences pituitary-thyroid axis regulation, with deficiency increasing TSH synthesis and enlarging the thyroid. Supplementation with 200,000 IU vitamin A improved goiter rates in combined deficiency states. Zinc plays roles in optimal T3, T4, and TSH levels, with deficiency associated with thyroid dysfunction.
Distinguishing Adaptation from Pathology Guides Clinical Decisions
The ability to differentiate normal physiological adaptation from pathological responses determines appropriate clinical management. Normal adaptation presents with TSH below 4.5 mU/L, absence of symptoms, normal free T4 and T3 levels, stabilization within 3-6 months, and stable thyroid antibody levels. The trajectory shows initial elevation followed by stabilization, responding appropriately to continued iodine optimization.
Pathological responses demonstrate progressive TSH elevation often exceeding 10 mU/L, declining free T4 levels indicating overt hypothyroidism, development of clinical symptoms, frequently positive or rising TPO/TgAb antibodies, and a progressive course without treatment. The trajectory shows continued worsening rather than stabilization, requiring thyroid hormone replacement therapy rather than simple iodine adjustment.
Key distinguishing features guide clinical decision-making. The trajectory differentiates conditions: adaptation shows stabilization while true hypothyroidism progresses. Symptoms separate them clearly: adaptation remains asymptomatic while true hypothyroidism causes clinical manifestations. Free hormone levels stay normal in adaptation but decline in true hypothyroidism. Antibody levels remain stable during adaptation but often elevate or rise in true hypothyroidism.
Red flags requiring immediate attention include rapid TSH rises exceeding 50% within 4-6 weeks, development of hypothyroid symptoms, TSH exceeding 15 mU/L at any time, declining free T4 levels, or new or worsening goiter. These findings warrant immediate endocrinology consultation and consideration of thyroid hormone replacement therapy.
Conclusion
TSH elevation during iodine repletion represents a complex interplay of protective autoregulatory mechanisms designed to prevent thyroid hormone excess. While the Wolff-Chaikoff effect and subsequent adaptations typically resolve within weeks to months in healthy individuals, certain populations—particularly those with autoimmune thyroid disease, nodular goiter, advanced age, or pregnancy—face elevated risks of persistent dysfunction. Understanding these mechanisms, recognizing warning signs, and implementing appropriate monitoring protocols enables clinicians to distinguish normal adaptation from pathological responses, ensuring safe and effective iodine supplementation. The critical role of cofactors, especially selenium, and the importance of proper supplementation sequencing further emphasize the need for individualized, evidence-based approaches to iodine repletion.