For millions of women living with endometriosis, the search for effective treatments often feels endless. Emerging research and clinical experience suggest that iodine – an essential nutrient many of us lack – may offer significant relief from endometriosis symptoms through its effects on hormone balance, inflammation, and tissue healing. While more research is needed, the combination of scientific evidence, expert clinical experience, and compelling patient stories paints a hopeful picture for women seeking natural approaches to manage their condition.
The connection between iodine and endometriosis centers on a surprising fact: nearly 70% of women in countries like the UK and US are iodine deficient, and this deficiency may be directly contributing to the development and progression of endometriosis. Studies show that women with endometriosis have up to 5-fold higher levels of iodine transporters in their endometrial tissue, suggesting their bodies are desperately trying to absorb more of this crucial nutrient. When iodine levels are restored, many women experience dramatic improvements – from severe pain dropping to manageable levels, to some even canceling planned surgeries.
The Science Reveals Multiple Pathways to Healing
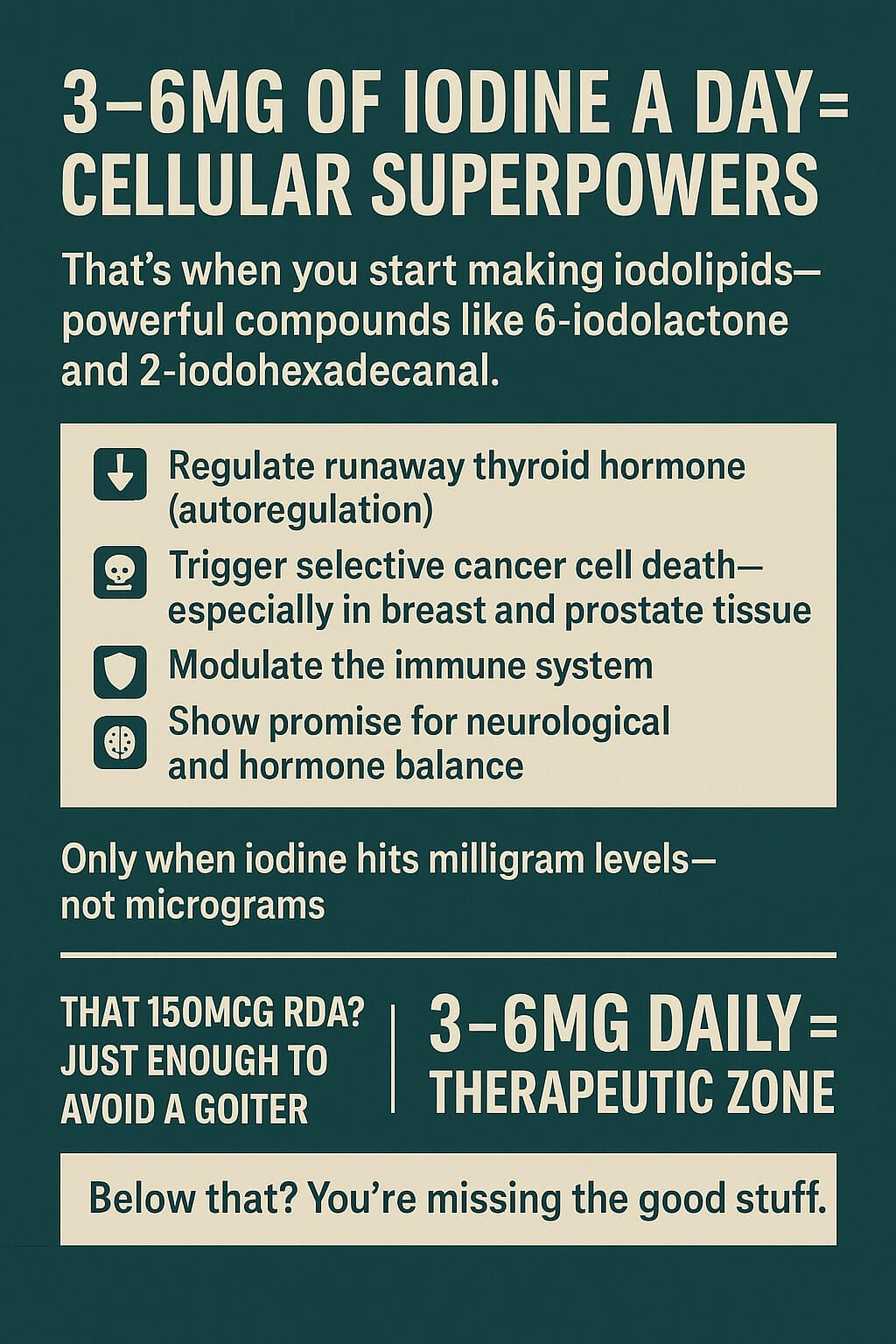
Research into iodine’s role in endometriosis has uncovered several mechanisms by which this nutrient may help. A groundbreaking Korean study analyzing over 1.7 million women found that endometriosis, fibrocystic breast disease, and thyroid problems often occur together – all linked by iodine deficiency. The researchers discovered that lack of iodine disrupts estrogen metabolism in two key ways: it reduces the activity of enzymes that break down estrogen (CYP1A1 and CYP1B1), and it decreases BRCA1 activity, leading to increased estrogen receptor activation.
Perhaps most intriguingly, studies using advanced imaging technology have found lower iodine levels in endometrial implants compared to normal tissue, with 98.8% accuracy in distinguishing between them. This suggests endometriosis might actually be, at least in part, an iodine deficiency disease. The Lipiodol studies, which used iodine-containing contrast medium, showed that women with endometriosis experienced a 5.4-fold increase in pregnancy rates within six months of treatment, though the effects were temporary without continued supplementation.
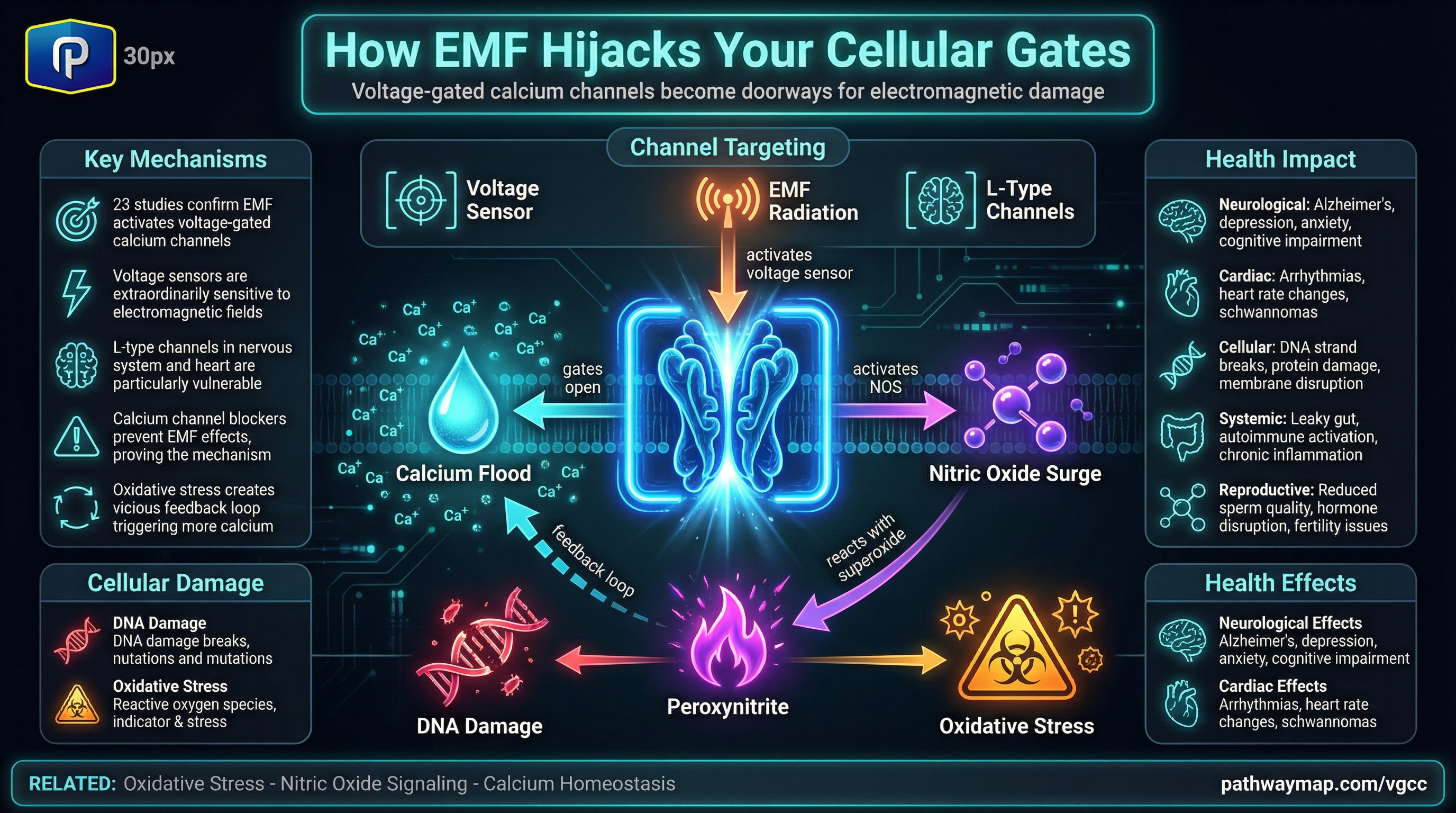
Iodine appears to work through multiple pathways simultaneously. It acts as a natural aromatase inhibitor, blocking the enzyme that converts other hormones into estrogen. It shifts estrogen metabolism away from the “strong” forms (estradiol and estrone) toward the protective “weak” form (estriol). Additionally, iodine has powerful anti-inflammatory and immune-modulating effects, addressing the chronic inflammation that characterizes endometriosis. Most remarkably, research shows that elemental iodine can actually dissolve fibrous tissue – a finding that has profound implications for breaking down endometrial implants and scar tissue.
Real Women, Real Results That Inspire Hope
The scientific evidence becomes even more compelling when combined with the experiences of women who have used iodine supplementation. One of Dr. Clearwoman’s UK patients saw her endometriosis pain drop from an unbearable 10 out of 10 to a manageable 3 out of 10 within six months of starting iodine therapy. She began with 3mg daily of Lugol’s iodine, gradually increasing to 50mg over several weeks, maintained that dose for 3-4 months, then reduced to 10mg daily for maintenance.
Elaina, whose endometriosis had spread from her pouch of douglas throughout her pelvis and onto her kidney over three years, recently began supplementing with bladderwrack (a seaweed high in iodine) after reading about the connection between iodine deficiency and endometriosis. She combines this with evening primrose oil, magnesium, probiotics, and vitamin B6 as part of a holistic approach to managing her condition.
Common patterns emerge from patient testimonials. Most women experience some initial detox symptoms – particularly vivid dreams and insomnia – for the first 2-3 weeks as iodine displaces bromine from their tissues. After this initial period, improvements typically include reduced pelvic pain, lighter and less painful periods, decreased pain during intercourse, and better overall energy. Many report that symptoms return when they stop supplementation but resolve again when they restart, confirming iodine’s role in their improvement.
The timeline for improvement varies, but most women notice initial changes within 2-4 weeks, with significant pain reduction by 3-6 months. Lucy Rose Clinic reports that some clients have even canceled planned surgeries due to their dramatic improvements. However, practitioners emphasize that success requires a comprehensive approach – iodine works best when combined with dietary changes, stress management, and addressing other nutritional deficiencies.
Leading Experts Weigh In With Decades of Clinical Experience
Dr. David Brownstein, who has treated thousands of patients with iodine over 20+ years, specifically identifies endometriosis as one of the conditions that responds well to iodine therapy. He explains that “iodine levels have fallen nearly 60% in the last 40 years, and during that same time period we have seen epidemic increases in hormone-related conditions including endometriosis.” His standard protocol starts patients at 25mg daily, adjusting based on individual response.
Dr. Guy Abraham, the UCLA professor who pioneered high-dose iodine research, documented cases where women with proven endometriosis experienced complete relief of pelvic pain within two menstrual cycles of starting elemental iodine therapy. His research revealed that 99% of the world population is deficient in iodine, and that this deficiency particularly affects hormone-sensitive tissues.
Dr. Lara Briden, a leading naturopathic hormone expert, recommends a more conservative approach of 1-3mg of molecular iodine daily for her endometriosis patients. She emphasizes that “iodine improves endometriosis because it’s anti-estrogenic, antimicrobial, and immune-modulating.” She always tests for thyroid antibodies first, as those with autoimmune thyroid conditions need to limit their intake to 300mcg daily.
The consensus among integrative practitioners is clear: iodine deficiency appears to be a significant contributing factor to endometriosis, and addressing this deficiency can lead to substantial improvements. However, they stress the importance of proper testing, appropriate dosing, and comprehensive support including companion nutrients like selenium, magnesium, and vitamin C.
Practical Guidance for Getting Started Safely
If you’re considering iodine supplementation for endometriosis, experts recommend starting with proper testing. A spot urine iodine test using the ICP-MS method provides the most accurate assessment of your current status. Equally important is testing thyroid antibodies (anti-TPO and anti-thyroglobulin), as those with positive antibodies need to follow a different, lower-dose protocol.
The most effective form for endometriosis appears to be elemental or molecular iodine (I₂), which has unique anti-estrogenic properties and can dissolve fibrous tissue. Lugol’s solution, containing both elemental iodine and potassium iodide, is the most commonly used and cost-effective option. A typical protocol might look like:
- Weeks 1-2: Start companion nutrients (200mcg selenium, 400mg magnesium, 1000mg vitamin C)
- Week 3: Begin with 3mg iodine daily
- Weeks 4-8: Gradually increase by 6mg weekly up to 25-50mg daily
- Months 2-4: Maintain therapeutic dose
- Month 4+: Reduce to 10mg daily maintenance
Essential companion nutrients protect the thyroid and optimize iodine utilization. Selenium is particularly crucial, as it prevents potential thyroid problems during supplementation. Taking these nutrients two weeks before starting iodine helps prepare your body for the protocol.
Safety considerations include watching for common side effects like metallic taste, temporary acne, or the “bromine detox” symptoms mentioned earlier. More serious concerns involve thyroid dysfunction, which is why regular monitoring is essential. Those who are pregnant, breastfeeding, or have autoimmune thyroid disease should work closely with a healthcare provider or avoid high-dose protocols entirely.
Integrating Iodine Into Your Broader Healing Journey
Successful management of endometriosis with iodine rarely happens in isolation. Practitioners emphasize the importance of a comprehensive approach that includes eliminating xenoestrogens from your environment (found in plastics, conventional personal care products, and pesticides), following an anti-inflammatory diet, managing stress, and supporting liver detoxification.
The connection between iodine and fertility deserves special mention. Studies show that correcting iodine deficiency can improve fertility in women with endometriosis, both through direct effects on the endometrium and by reducing inflammation in the reproductive system. The temporary fertility boost seen in the Lipiodol studies suggests that maintaining adequate iodine levels may be important for those trying to conceive.
Many women find that iodine works synergistically with other natural approaches. Some combine it with enzymes like nattokinase to help dissolve scar tissue, while others use it alongside bioidentical progesterone to balance hormones. The key is finding the right combination for your individual situation, ideally with guidance from a knowledgeable practitioner.
The Bigger Picture Offers Reasons for Optimism
The relationship between iodine and endometriosis represents a significant shift in how we might approach this challenging condition. Rather than simply managing symptoms, addressing iodine deficiency may help correct one of the underlying factors that allows endometriosis to develop and progress. The fact that women in iodine-sufficient populations like Japan have much lower rates of endometriosis supports this connection.
Current research gaps mean we don’t yet have large randomized controlled trials specifically testing iodine supplementation for endometriosis. However, the combination of mechanistic studies, clinical experience, and patient testimonials provides compelling evidence that this approach deserves serious consideration. The safety profile of iodine, when used appropriately with proper testing and monitoring, makes it a reasonable option to explore.
For women who have struggled with conventional treatments or are seeking natural approaches, iodine supplementation offers genuine hope. While not every woman will experience dramatic improvements, the potential benefits – from significant pain reduction to improved fertility – make it worth investigating with appropriate medical guidance.
Your Path Forward Starts With Small Steps
If you’re intrigued by the potential of iodine for your endometriosis, remember that healing is a journey, not a destination. Start by getting your iodine levels tested and finding a practitioner familiar with iodine protocols. Be patient with the process – while some women experience rapid improvements, others need several months to see significant changes.
Most importantly, remember that you’re not alone in this journey. The growing community of women successfully using iodine for endometriosis, combined with increasing practitioner awareness and ongoing research, suggests that better days may be ahead. Whether iodine becomes part of your healing protocol or not, the fact that researchers and clinicians are uncovering new connections and treatment options offers hope for all women living with endometriosis.
The message from both science and real-world experience is clear: addressing iodine deficiency may be a missing piece of the endometriosis puzzle for many women. With proper testing, appropriate supplementation, and comprehensive support, this essential nutrient offers a promising path toward reduced pain, improved hormonal balance, and better quality of life. While we await more definitive research, the current evidence suggests that for many women with endometriosis, ensuring adequate iodine levels may be one of the most important steps they can take on their healing journey.