The Biochemistry of Histamines and Iodine Supplementation
We’re looking at why iodine can ‘stir up’ histamines. The idea is that iodine kicks off detox, which moves around the same irritants that randomly set off histamine in the first place.
Histamine reactions during iodine supplementation represent a complex interplay of detoxification, cellular rebalancing, and metabolic shifts. The primary mechanism involves bromide displacement from tissues triggering temporary mast cell instability, while multiple secondary pathways contribute to what practitioners describe as “moving histamines around” – a redistribution of histamine from tissue-bound stores into circulation before eventual clearance.
Histamine’s Fundamental Biochemistry
Histamine (C₅H₉N₃) consists of an imidazole ring attached to an ethylamine chain, a deceptively simple structure that enables remarkable biological versatility. This small molecule, weighing just 111.15 g/mol, exists as a monoprotonated cation at physiological pH, with its imidazole ring providing unique tautomeric properties that allow binding to multiple receptor types.
The body produces histamine primarily in mast cells and basophils for immune responses, enterochromaffin-like cells in the stomach for gastric acid regulation, and histaminergic neurons in the hypothalamus for neurotransmission. The synthesis pathway is elegantly simple: the enzyme histidine decarboxylase (HDC) removes a carboxyl group from L-histidine, requiring only pyridoxal phosphate as a cofactor. This single enzymatic step, occurring at highest rates in the gallbladder, stomach, and lungs, produces a molecule that participates in at least 23 distinct physiological functions.
Beyond its well-known role in allergic reactions, histamine serves as a critical regulator of gastric acid secretion, a neurotransmitter controlling sleep-wake cycles, and a modulator of vascular permeability. The body maintains tight control over histamine levels through two primary degradation pathways: diamine oxidase (DAO) handles extracellular histamine primarily in the gut, while histamine N-methyltransferase (HNMT) processes intracellular histamine, particularly in the central nervous system. These enzymes typically clear histamine within 1-10 minutes of release, highlighting the molecule’s potent but transient nature.
Four Receptors Create Diverse Symptom Patterns
Histamine’s diverse effects arise from its interaction with four distinct G-protein coupled receptors, each triggering unique cellular responses and symptoms. Understanding these receptor-specific effects explains why histamine reactions can manifest so differently between individuals.
H1 Receptors Drive Classic Allergic Symptoms
H1 receptors, distributed throughout smooth muscle, vascular endothelium, and sensory nerves, couple to Gq/11 proteins that activate phospholipase C and mobilize intracellular calcium. When activated, these receptors produce the familiar cascade of allergic symptoms: itching, sneezing, runny nose, watery eyes, and hives. In the airways, H1 activation causes bronchoconstriction, while in blood vessels it increases permeability leading to tissue swelling and edema. The separation of endothelial cells creates the characteristic wheals and flares of allergic skin reactions. Second-generation H1 antagonists like cetirizine and loratadine effectively block these receptors without crossing the blood-brain barrier, avoiding the sedation caused by first-generation drugs like diphenhydramine.
H2 Receptors Control Acid Secretion and Heart Rate
H2 receptors predominantly occupy gastric parietal cells where they regulate stomach acid production through the Gs protein-adenylyl cyclase-cAMP pathway. This signaling cascade activates the H⁺/K⁺-ATPase proton pumps, resulting in hydrochloric acid secretion at an impressive concentration of 160 mM (pH 0.8). Beyond the stomach, H2 receptors in cardiac tissue cause tachycardia and increased contractility, while those in blood vessels contribute to vasodilation. The combination of H1 and H2 activation explains the hypotension and flushing seen in severe allergic reactions. Famotidine remains the preferred H2 blocker due to minimal drug interactions, though the entire class has revolutionized peptic ulcer treatment.
H3 Receptors Modulate Neurotransmitter Release
H3 receptors function primarily as presynaptic autoreceptors and heteroreceptors in the central nervous system, particularly concentrated in the tuberomammillary nucleus. Through Gi/o protein coupling, they inhibit adenylyl cyclase and reduce calcium channel activity, thereby decreasing neurotransmitter release. This creates a feedback mechanism controlling histamine synthesis while also modulating release of dopamine, serotonin, norepinephrine, acetylcholine, GABA, and glutamate. Unlike other histamine receptors, H3 shows constitutive activity even without histamine binding. These receptors regulate sleep-wake cycles, cognitive function, and appetite, with pitolisant representing the first approved H3 antagonist for narcolepsy treatment.
H4 Receptors Orchestrate Inflammation
H4 receptors, discovered most recently, express primarily on immune cells including mast cells, eosinophils, basophils, and T cells. Like H3, they couple to Gi/o proteins but uniquely mediate immune cell chemotaxis and inflammatory mediator release. H4 activation recruits eosinophils and mast cells to inflammatory sites, enhances cytokine production, and promotes T cell differentiation toward the Th2 phenotype associated with allergic responses. These receptors show particular promise as therapeutic targets for chronic inflammatory conditions like atopic dermatitis and inflammatory bowel disease, though selective antagonists remain in development.
Why Iodine Triggers Histamine Mobilization
The connection between iodine supplementation and histamine reactions involves multiple interconnected mechanisms, with halogen displacement serving as the primary driver. When supplemental iodine enters the body, it preferentially binds to iodine receptors throughout various tissues, displacing other halogens—particularly bromide—that have accumulated over years of environmental exposure.
Bromide Displacement Creates Temporary Chaos
Modern environmental exposure to bromide through flame retardants, pesticides, and brominated flour has created unprecedented tissue accumulation. Dr. David Brownstein’s research documented that breast cancer patients had 50% higher bromide levels and 50% lower iodine levels compared to healthy controls. When iodine supplementation begins, it displaces bromide in approximately a 1:1 ratio from thyroid, breast, prostate, and other tissues. This sudden mobilization of bromide into circulation triggers what was historically misdiagnosed as “iodism” but is actually “bromism”—bromide toxicity from displacement.
The released bromide destabilizes mast cells, causing degranulation and histamine release. This explains why initial supplementation symptoms—skin rashes, brain fog, anxiety, metallic taste—closely mimic histamine intolerance reactions. Studies confirm that bromide exposure can directly trigger histamine release from mast cells, creating a constellation of symptoms that typically peaks during the first 2-8 weeks of supplementation as the body works to excrete accumulated bromide through kidneys and sweat.
Dual Effects on Mast Cell Stability
Research reveals a fascinating paradox: iodine shows both stabilizing and destabilizing effects on mast cells depending on its form and concentration. Molecular iodine (I₂) demonstrates mast cell stabilizing properties, inhibiting degranulation in non-infectious cell damage models and decreasing neutrophil chemotaxis. Studies using iodine-enriched eggs found dose-dependent inhibition of histamine release from rat mast cells, with the active compounds concentrated in neutral lipid fractions.
Conversely, iodinated contrast media and high-dose iodine cause dose-dependent histamine release from basophils and mast cells. These compounds can activate MRGPRX2 receptors on mast cells, leading to pseudo-allergic reactions. Ionic iodine compounds prove more potent mast cell activators than non-ionic forms, showing biphasic histamine release responses at higher concentrations. This dual nature explains why some individuals experience immediate relief while others face initial worsening of histamine symptoms.
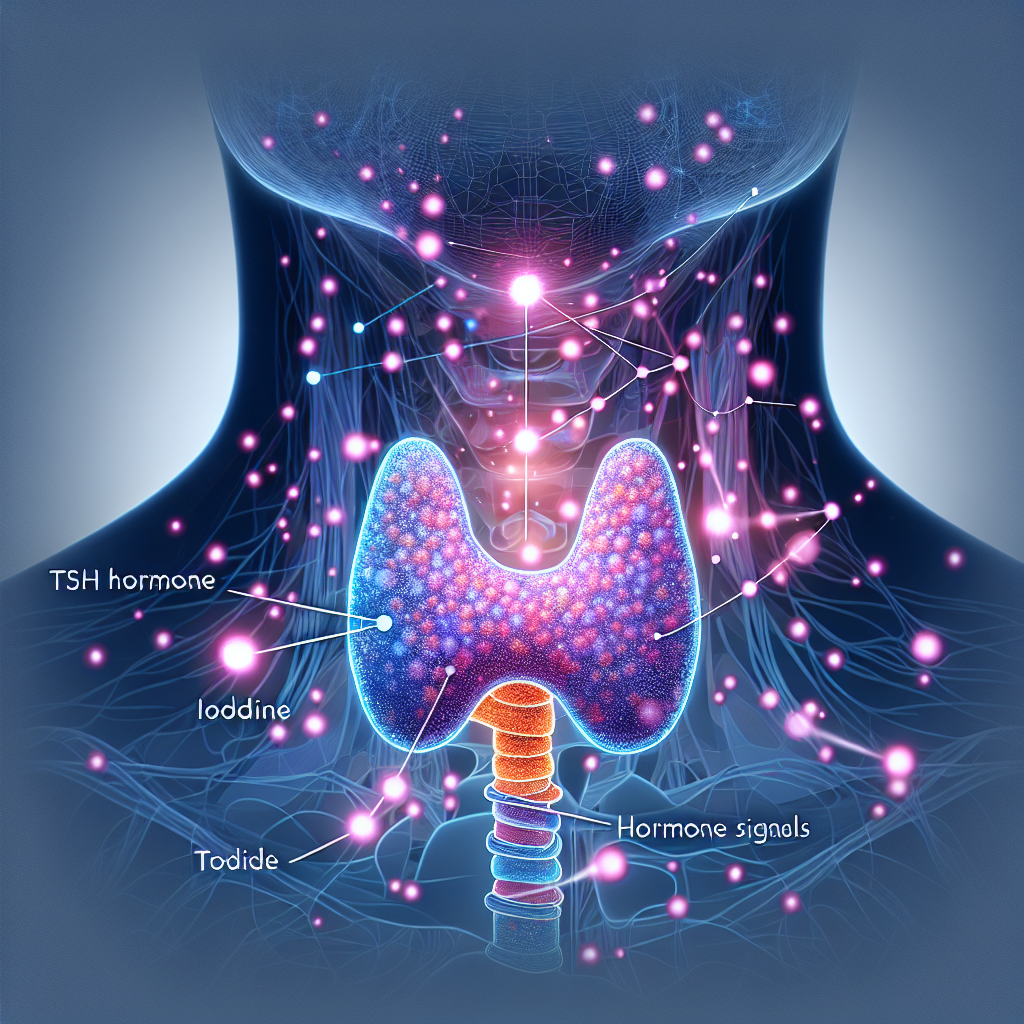
Thyroid-Histamine Bidirectional Relationship
The thyroid-histamine connection operates bidirectionally: low thyroid function increases histamine production while high thyroid function increases histamine receptor sensitivity. T3 directly increases histamine concentration in the hypothalamus, thalamus, and cerebral cortex. Mast cells themselves possess receptors for T3 and TSH, can store thyroid hormones, and their numbers in tissues are regulated by thyroid hormone levels.
This relationship becomes particularly relevant in Hashimoto’s thyroiditis, where patients frequently develop histamine intolerance. T3 supplementation can cause systemic itching through histamine-dependent pathways, while histamine can interfere with iodine uptake by competing for thyroid transporters. The complex interplay suggests that optimizing thyroid function through iodine supplementation may temporarily disrupt histamine balance before ultimately improving it.
Detoxification Pathway Overload
High-dose iodine supplementation simultaneously activates multiple detoxification pathways, creating a temporary metabolic storm. As iodine mobilizes stored toxins from fat-soluble tissues, the liver becomes overwhelmed processing displaced halogens. Phase II detoxification pathways require substantial cofactors—magnesium, selenium, B vitamins—and insufficient availability leads to incomplete detoxification with toxic metabolite accumulation.
This overwhelmed detoxification creates oxidative stress that triggers mast cell activation and histamine release. Liver congestion impairs histamine clearance while gut inflammation from detox byproducts increases intestinal permeability, allowing more histamine to enter circulation. The “moving histamines around” phenomenon practitioners observe represents this redistribution: histamine released from tissue-bound stores, mobilized from degranulating mast cells, and shifted from intracellular to extracellular compartments where it causes symptoms before eventual clearance.
Clinical Evidence Shapes Treatment Protocols
Leading practitioners have developed sophisticated protocols based on decades of clinical observation and emerging research. Dr. Guy Abraham’s Iodine Project challenged “medical iodophobia” by demonstrating that most people require significantly more iodine than the current RDA of 150 mcg. Historical precedent supports this: between 1900-1960s, physicians routinely prescribed 12.5-37.5 mg daily of Lugol’s solution without significant adverse effects.
The Salt Loading Breakthrough
The salt loading protocol represents a crucial innovation for managing histamine-like detox symptoms. Mixing 1/4 to 1/2 teaspoon of unrefined sea salt in warm water, followed by 10-12 ounces of pure water, helps bind and eliminate bromide through the kidneys. The chloride in salt binds to bromide in the bloodstream, enhancing elimination while providing essential electrolyte support during detoxification. Practitioners report this simple intervention often provides relief within 30-45 minutes of administration.
Dr. Brownstein’s standard protocol starts patients at 25 mg daily, increasing to 50+ mg for endocrine diseases, always accompanied by essential companion nutrients. These include selenium (200-400 mcg) to prevent thyroid damage, magnesium (400-1200 mg) to support detox pathways, vitamin C (3,000-10,000 mg) for antioxidant protection, and B-vitamins including riboflavin and niacin as ATP cofactors. Pre-treatment with these nutrients for 1-2 weeks before starting iodine significantly reduces adverse reactions.
Emerging Research on Ferroptosis
Recent groundbreaking research published in Nature Scientific Reports (2023) reveals that lecithin-bound iodine induces ferroptosis in activated B cells, suppressing allergen-specific IgE production. This iron-dependent programmed cell death pathway represents a novel mechanism by which iodine modulates immune responses. Potassium iodide increases intracellular reactive oxygen species and ferrous iron, leading to ferroptosis in activated B cells and T follicular helper cells that contribute to allergic responses.
This discovery suggests that initial immune system rebalancing from iodine could temporarily increase inflammatory mediator release, including histamine, before ultimately reducing allergic sensitivity. The study noted that effects on mast cells remain unknown, highlighting an important area for future research.
Individual Variation Determines Response
Not everyone experiences histamine reactions during iodine supplementation, and severity varies dramatically based on multiple factors. Genetic polymorphisms in DAO enzyme (AOC1 gene variations) and methylation pathways (MTHFR variants) significantly impact histamine metabolism. Those with existing mast cell activation syndrome show heightened reactivity, while individuals with high baseline toxin loads experience more intense displacement reactions.
Gut health plays a crucial role: SIBO, leaky gut, and dysbiosis worsen histamine reactions by compromising DAO production and increasing intestinal permeability. Methylation capacity affects detoxification ability, with MTHFR and other genetic variants creating bottlenecks in histamine clearance pathways. The form of iodine matters too—molecular iodine (I₂) typically causes fewer reactions than iodide (I⁻) forms.
Cofactor status proves critical for successful supplementation. Deficiencies in magnesium, selenium, B vitamins, and vitamin C not only increase reaction severity but may prevent the therapeutic benefits of iodine repletion. Clinical observations suggest that symptoms typically resolve within 2-8 weeks when proper support is provided, with many patients reporting improved energy, mental clarity, and reduced allergy symptoms after the initial adjustment period.
Conclusion
The iodine-histamine connection represents a temporary but significant challenge in correcting iodine deficiency. Understanding the underlying mechanisms—primarily bromide displacement triggering mast cell instability—allows practitioners to design protocols that minimize adverse reactions while achieving therapeutic benefits. The phenomenon of “moving histamines around” describes a complex redistribution process as the body rebalances after years of halogen accumulation and iodine deficiency.
Success requires a comprehensive approach: gradual dose titration, essential companion nutrients, salt loading for bromide elimination, and patience during the initial adjustment period. For individuals with histamine intolerance, addressing iodine status may provide unexpected benefits, though the path to improvement often involves navigating temporary symptom exacerbation. As research continues to elucidate these mechanisms, particularly regarding direct mast cell effects and optimal dosing strategies, clinicians gain increasingly sophisticated tools for managing this complex therapeutic challenge.
Read More
Iodine and histamines is just one angle of histamines. I also more about histamines in general here /histamines