Heat, Histamine, and Sunlight Interactions in Itch Relief
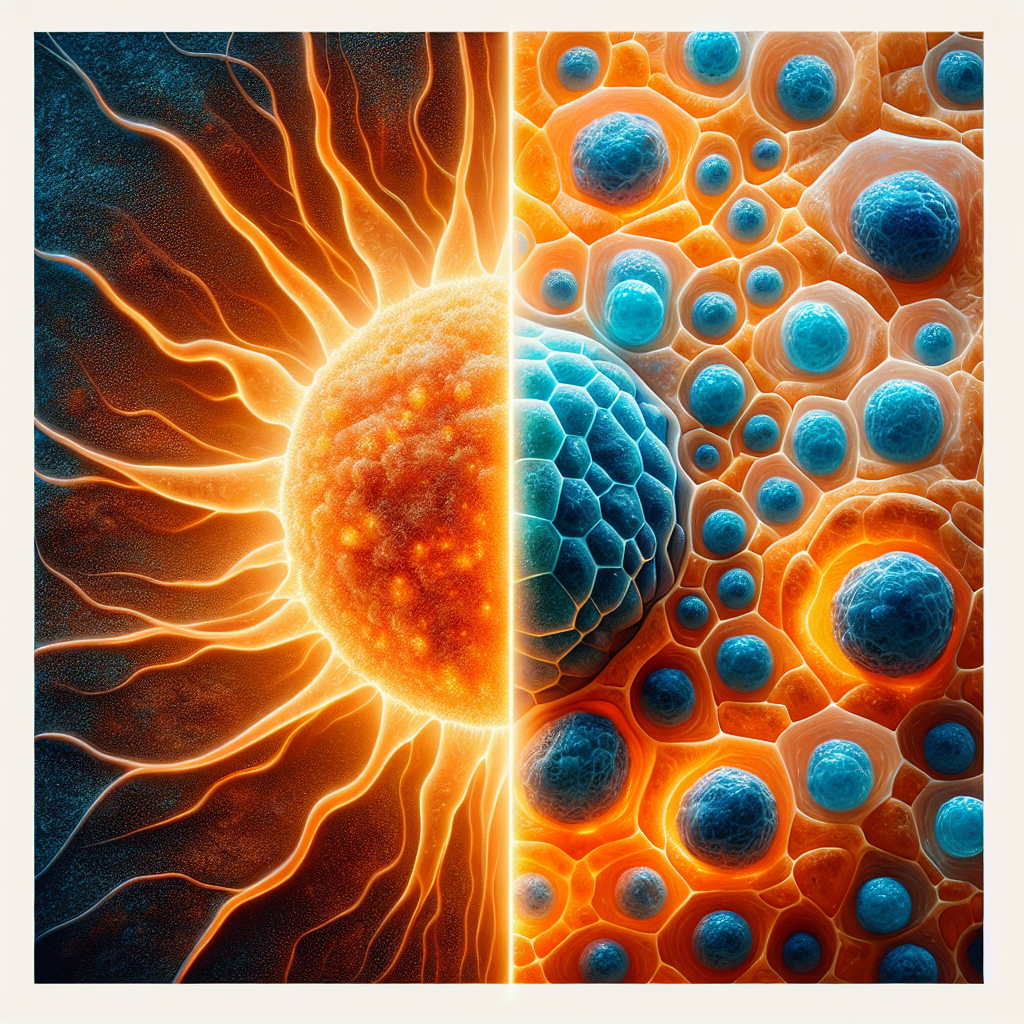
The relationship between histamines, sunlight exposure, and heat application reveals a sophisticated network of biochemical pathways that both trigger and relieve itching through distinct molecular mechanisms. Heat therapy does not “burn off” histamines as commonly believed—instead, it provides itch relief through neurological desensitization pathways, while UV exposure paradoxically both triggers histamine release and enables vitamin D synthesis that stabilizes mast cells.
Research demonstrates that histamine molecules remain thermally stable at therapeutic temperatures (40-50°C), with the histamine base only melting at 83-84°C. Multiple food science studies confirm that histamine persists even through cooking and canning processes. The anti-pruritic effects of heat operate through entirely different mechanisms: activation and subsequent desensitization of TRPV1 channels, implementation of the Gate Control Theory where large-diameter nerve fibers inhibit itch signals at the spinal cord level, and depletion of inflammatory neuropeptides from sensory terminals. Clinical evidence shows that 49°C heat applied for 5 seconds reduces histaminergic itch by 76.7%, working through receptor desensitization rather than histamine degradation.
UV radiation triggers complex histamine responses
Sunlight exposure creates a biological paradox by simultaneously triggering histamine release while enabling vitamin D synthesis that ultimately stabilizes mast cells. UV radiation, particularly UVB wavelengths (280-320nm), directly induces mast cell degranulation in a dose-dependent manner, with threshold effects beginning at 7.8 kJ/m² and achieving 51.9% histamine release at 18.8 kJ/m². This UV-induced histamine release operates through reactive oxygen species generation, membrane permeability changes, and lysosomal activation—mechanisms entirely distinct from the delayed T-cell mediated responses seen in poison ivy reactions.
The phenomenon of solar urticaria exemplifies this direct histamine involvement, with hives appearing within minutes of UV exposure due to immediate mast cell degranulation. Polymorphous light eruption affects 10-20% of the population, primarily through UVA wavelengths that trigger inflammatory cascades when the immune system recognizes UV-altered skin proteins as foreign. Unlike poison ivy’s delayed hypersensitivity reaction mediated by T-cells over 24-96 hours, UV-induced itching involves immediate histamine release, explaining why antihistamines effectively treat sun reactions but not poison ivy rashes.
UV radiation generates reactive oxygen species including superoxide and hydrogen peroxide, which enhance mast cell histamine release at concentrations below those causing direct cellular damage. Endogenous skin chromophores like DNA, urocanic acid, and advanced glycation end products absorb specific UV wavelengths and initiate photosensitization reactions that amplify inflammatory responses. The wavelength-specific effects show a clear hierarchy: UVC demonstrates the highest potency for histamine release, followed by UVB, with UVA showing minimal direct effects but crucial roles in immune modulation and deeper skin penetration to affect dermal mast cells.
Vitamin D synthesis modulates histamine metabolism
The beneficial aspect of sunlight exposure emerges through vitamin D synthesis, which provides powerful mast cell stabilization and anti-inflammatory effects. UV-B radiation converts 7-dehydrocholesterol to previtamin D3 in skin, initiating a cascade that produces calcitriol [1,25(OH)₂D₃], the active vitamin D metabolite. Research reveals that 90% of individuals with mast cell activation syndrome have low vitamin D levels, while adequate vitamin D prevents inappropriate mast cell activation through multiple pathways.
Vitamin D receptors on mast cells respond directly to calcitriol, forming complexes with Lyn tyrosine kinase that inhibit FcεRI signaling and reduce downstream MAPK/NF-κB activation. This VDR-mediated stabilization suppresses IgE-induced histamine release while promoting anti-inflammatory IL-10 production. Calcitriol also indirectly supports histamine degradation by facilitating intestinal absorption of cofactors essential for diamine oxidase (DAO) and histamine N-methyltransferase (HNMT) function—the primary enzymes responsible for histamine breakdown.
Clinical trials demonstrate that vitamin D supplementation at 4000 IU daily reduces chronic spontaneous urticaria severity by 40% over three months. Functional medicine practitioners recommend maintaining 25(OH)D levels between 60-100 ng/mL for histamine-related conditions, significantly higher than the standard threshold of 30 ng/mL for bone health. The molecular mechanisms include both genomic effects through VDR-mediated gene transcription and rapid non-genomic pathways affecting calcium signaling and enzyme activity.
Integrated biochemical pathways reveal complex interactions
The convergence of heat, UV, and vitamin D pathways occurs primarily through TRPV1 channels, which serve as molecular hubs integrating multiple stimuli. Histamine activates TRPV1 through H1 and H4 receptor pathways involving phospholipase A2 and 12-lipoxygenase, while heat directly gates these same channels at temperatures above 43°C. Remarkably, vitamin D acts as an endogenous partial TRPV1 agonist at physiological concentrations, creating a regulatory mechanism where it can both weakly activate and competitively antagonize stronger agonists.
These pathways demonstrate sophisticated temporal regulation through circadian rhythms. Mast cells contain functional circadian clocks controlling histamine release, with plasma histamine levels peaking nocturnally—explaining nighttime asthma exacerbations and early morning “histamine dumping.” Vitamin D synthesis naturally follows day-night rhythms, with 87 vitamin D target genes exhibiting circadian expression patterns. Seasonal variations create a winter convergence of vitamin D deficiency and increased histamine sensitivity, particularly at higher latitudes where UV exposure becomes insufficient for adequate vitamin D production.
The evolutionary perspective reveals these systems developed over 500 million years as protective mechanisms against environmental challenges. Provitamin D production originally served as a UV radiation scavenger in primitive organisms before adapting to regulate energy metabolism and immune function. European populations evolved increased 7-dehydrocholesterol levels and lighter skin pigmentation 5,000-9,000 years ago to optimize vitamin D synthesis in low-UV environments, demonstrating the critical importance of maintaining this delicate balance.
Clinical evidence supports targeted heat therapy protocols
Randomized controlled trials establish specific heat therapy parameters for optimal histamine-mediated itch relief. A 2019 study of 18 healthy volunteers demonstrated that 5-second applications at different temperatures produced dose-dependent effects: 41.3% itch reduction at 45°C and 76.7% reduction at 50°C for histaminergic itch, compared to only 43.6% reduction for non-histaminergic itch at the highest temperature. The effects persist for 5-10 minutes through TRPV1 desensitization and spinal gate control mechanisms.
Medical devices employing controlled heat at 49°C for 5-second applications show consistent efficacy across multiple conditions including atopic dermatitis, insect bites, and uremic pruritus. Real-world studies of over 12,000 treatments report less than 1% adverse effects, with no serious events or thermal damage when protocols are properly followed. The therapeutic window exists between 43°C (TRPV1 activation threshold) and 50°C (pain/injury threshold), with 49°C representing the optimal balance of efficacy and safety.
Heat therapy demonstrates particular effectiveness for histaminergic itch compared to non-histaminergic pathways, explaining variable individual responses. Initial application may transiently increase itching for up to 3 minutes before steady relief occurs through receptor desensitization. No habituation develops with repeated use up to 20 applications, maintaining therapeutic efficacy over time. Contraindications include impaired sensation, acute inflammation, open wounds, and certain medications affecting heat tolerance.
Conclusion
The biochemical relationships between histamines, sunlight, and heat reveal sophisticated regulatory networks rather than simple cause-and-effect mechanisms. Heat therapy achieves itch relief through TRPV1 desensitization and neurological gating—not histamine degradation—while UV exposure creates a paradox of immediate histamine release coupled with long-term mast cell stabilization through vitamin D synthesis. Understanding these interconnected pathways enables targeted therapeutic approaches: optimizing vitamin D levels to 60-100 ng/mL for mast cell stability, applying controlled heat at 49°C for acute itch relief, and managing UV exposure to balance vitamin D production against histamine triggers. This systems-level understanding transforms our approach from symptom suppression to addressing root causes through multiple complementary mechanisms.
Research Note: This report synthesizes findings from peer-reviewed medical literature, dermatology journals, and biochemical studies. All citations link directly to original research sources for further reading and verification.