Recent research reveals a profound connection between fat metabolism and our ability to handle sunlight exposure. When fat digestion and bile flow are compromised, people develop mysterious sun sensitivity that goes far beyond simple sunburn. Understanding these connections can help identify whether your light sensitivity might actually signal underlying metabolic issues.
How Fat Tissue Defends Against Sunlight
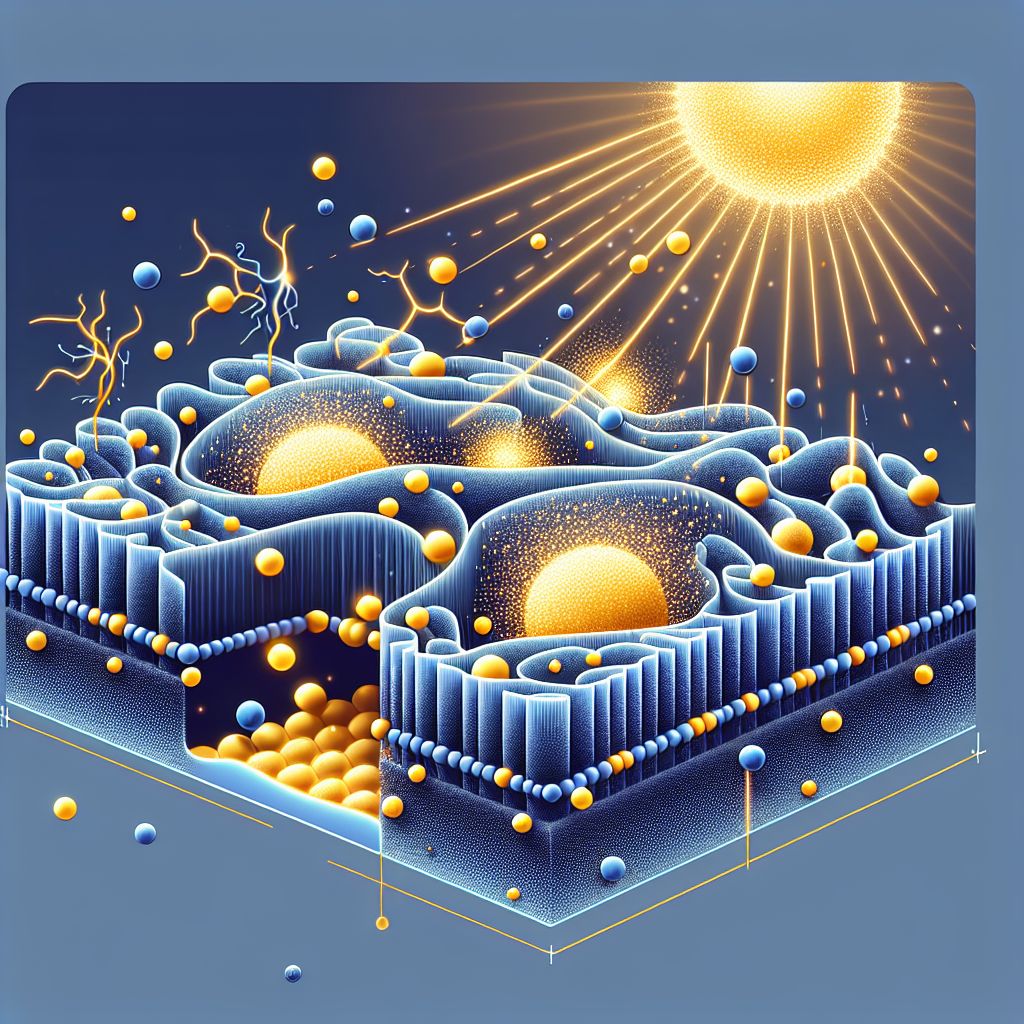
Fat doesn’t just store energy – it functions as a sophisticated light defense system through multiple mechanisms. While UV radiation cannot directly penetrate subcutaneous fat layers, fat tissue provides crucial photoprotection through optical scattering properties that modify how light travels through skin. More importantly, fat serves as the body’s primary storage depot for fat-soluble vitamins A, D, E, and K – all essential for UV defense.
Vitamin E, stored primarily in fat tissue, acts as the body’s main lipid-phase antioxidant, neutralizing free radicals generated by UV exposure. Vitamin A and carotenoids absorb specific wavelengths of light and reduce UV-induced skin damage by up to 60%. Vitamin D, synthesized in skin from UV exposure, requires fat for proper storage and distribution throughout the body. Without adequate fat metabolism, these protective systems fail, leaving skin vulnerable to light damage even from minimal exposure.
The relationship extends deeper than vitamins. Research shows that subcutaneous fat tissue contains light-sensitive signaling pathways – including melanopsin receptors that respond to blue light. When fat metabolism is disrupted, these light-sensing systems malfunction, creating abnormal responses to normal light exposure.
The Bile Flow Connection to Sun Sensitivity
Bile acids are essential for absorbing dietary fats and fat-soluble vitamins. When bile flow is compromised – through gallbladder disease, liver dysfunction, or bile acid malabsorption – fat-soluble vitamin deficiencies develop rapidly. This condition affects over 1% of the population but is frequently undiagnosed, with approximately 30% of patients diagnosed with “functional diarrhea” actually having bile acid malabsorption.
The clinical manifestations are striking. Vitamin E deficiency eliminates the primary antioxidant protection in skin cell membranes, making them extremely vulnerable to UV damage. Vitamin A deficiency compromises the skin barrier and reduces tear production, creating eye sensitivity to bright light. The result is a constellation of symptoms that people rarely connect to digestive issues: rapid sunburning despite normal skin tone, unusual fatigue after sun exposure, and eye discomfort in bright conditions.
More severe bile flow problems can cause accumulation of photosensitive compounds like porphyrins and phylloerythrin. These molecules act as photosensitizers – they absorb light energy and transfer it to surrounding tissues, causing damage within minutes of sun exposure. This explains why some liver disease patients develop severe photosensitivity that seems disproportionate to their sun exposure.
Common Symptoms of Fat Metabolism Issues You Might Not Recognize
Many people with fat metabolism dysfunction experience symptoms they never connect to their condition. Rapid sunburning that occurs faster than expected for your skin type often signals depleted fat-soluble antioxidants. This isn’t just sensitive skin – it’s biochemical vulnerability from missing protective nutrients.
Unusual fatigue after sun exposure represents more than simple heat exhaustion. When fat metabolism is compromised, cells cannot properly process light energy or repair UV damage, creating profound metabolic stress. The body attempts to repair damage without adequate resources, leading to exhaustion that persists long after sun exposure ends.
Eye symptoms are particularly revealing. Beyond simple brightness discomfort, people may experience photophobia (pain from light), dry eyes that worsen in bright conditions, or difficulty adapting between light and dark environments. These symptoms reflect vitamin A deficiency affecting rhodopsin production and tear film quality.
Atypical skin reactions include burning sensations without visible sunburn, skin that remains sensitive long after exposure, or reactions to minimal light through windows or on cloudy days. Some people develop skin changes from fluorescent lighting or computer screens – a sign that even non-UV wavelengths are triggering abnormal responses.
Light-triggered headaches represent another overlooked connection. Research shows migraines often reflect cerebral energy deficiency, with light exposure creating metabolic demands the brain cannot meet. When fat metabolism is impaired, the brain lacks adequate energy substrates, making light a migraine trigger.
Emerging Research on Light, Metabolism, and Eye Problems
Groundbreaking research is revealing that many eye problems previously blamed on aging or genetics actually stem from disrupted light-metabolism interactions. Macular degeneration, once thought primarily age-related, shows massive dysregulation of lipid metabolism genes. Clinical trials using modified vitamin A that resists toxic transformation have reduced disease progression by 21%, proving the fundamental role of fat metabolism in eye health.
Visual snow syndrome – seeing static or snow in the visual field – links to specific genetic variants affecting lipid metabolism, particularly the APOB gene. Patients show disrupted energy processing in brain regions that handle both visual information and metabolic regulation. Their symptoms worsen with blue light exposure, suggesting fundamental problems with how cells process light energy.
The retina contains the highest concentration of DHA (omega-3 fatty acid) in the body – over 50% of photoreceptor membrane lipids. This makes vision exquisitely dependent on fat metabolism. Poor omega-3 status increases light sensitivity, reduces visual performance, and accelerates age-related eye changes. Yet most eye doctors never assess patients’ fat absorption capacity.
Perhaps most striking is the discovery that fat cells themselves contain light receptors. Subcutaneous fat expresses opsin 3 (OPN3) photoreceptors that directly sense blue light and trigger metabolic responses. This means our fat tissue is actively processing light information – when this system fails, it disrupts energy metabolism, hormone production, and circadian rhythms.
Sunlight as a Nutrient Requiring Metabolic Processing
The emerging paradigm treats sunlight not just as something to block, but as an essential “nutrient” the body must properly process. Dr. Gerald Pollack’s research shows that infrared light from the sun structures cellular water into a fourth phase that stores energy and powers cellular processes. This requires healthy cell membranes rich in properly functioning lipids.
Red and near-infrared light directly stimulate mitochondrial ATP production – but only when mitochondrial membranes contain the right lipid composition. Studies show that people with metabolic dysfunction have reduced response to therapeutic light exposure. Their cells literally cannot “digest” light properly due to damaged membranes and depleted cofactors.
Circadian biology research reveals that 15% of metabolites in our blood follow light-dark cycles, with most being lipid metabolites. Fat tissue contains autonomous circadian clocks that respond to light exposure patterns. When bile flow problems disrupt fat metabolism, these timing systems fail, creating cascading effects on sleep, mood, and energy levels.
The clinical implications are profound. Rather than simply taking antioxidant supplements or using stronger sunscreen, addressing the root cause – impaired fat metabolism – can restore the body’s natural light processing abilities. This might involve treating bile acid malabsorption, optimizing liver function, or using targeted lipid replacement therapy to repair cellular membranes.
Recognizing if You Have Fat Metabolism Issues
Several patterns suggest fat metabolism problems might underlie your sun sensitivity. First, digestive symptoms often precede light sensitivity – chronic diarrhea, floating stools, or discomfort after fatty meals may indicate poor fat absorption. Second, multiple seemingly unrelated symptoms cluster together – if you have light-triggered headaches AND dry eyes AND unusual fatigue after sun exposure, consider metabolic causes.
Family history provides clues too. Gallbladder disease, liver problems, inflammatory bowel conditions, or celiac disease in relatives increases your risk. Previous gallbladder removal, gastric bypass surgery, or chronic use of bile acid sequestrants (cholesterol medications) directly impair fat absorption.
Blood tests can confirm suspicions. Low levels of vitamins A, D, E, or K despite adequate dietary intake suggest absorption problems. Elevated liver enzymes, abnormal lipid profiles, or inflammatory markers often accompany fat metabolism dysfunction. Specialized tests like SeHCAT scanning can diagnose bile acid malabsorption, though these aren’t widely available.
The key insight is recognizing that sun sensitivity isn’t just about skin type or sun protection habits. When fat metabolism fails, we lose our fundamental ability to process light as a nutrient and defend against its harmful effects. By understanding these connections, people can identify the true cause of their light sensitivity and pursue treatments that address the metabolic root rather than just managing symptoms.
Conclusion
Fat tissue serves as our body’s primary sunlight defense system – not through direct UV absorption, but through storing protective nutrients, maintaining cellular membranes, and enabling proper light energy processing. When bile flow problems compromise fat metabolism, this entire defense network collapses, creating mysterious sun sensitivity and light-related symptoms that seem unconnected to digestion.
Recognizing these patterns empowers people to look beyond surface-level sun protection to address underlying metabolic dysfunction. The emerging science suggests that restoring healthy fat metabolism might not only reduce sun sensitivity but also improve energy, mood, and overall vitality by enabling our bodies to properly “digest” light as nature intended.